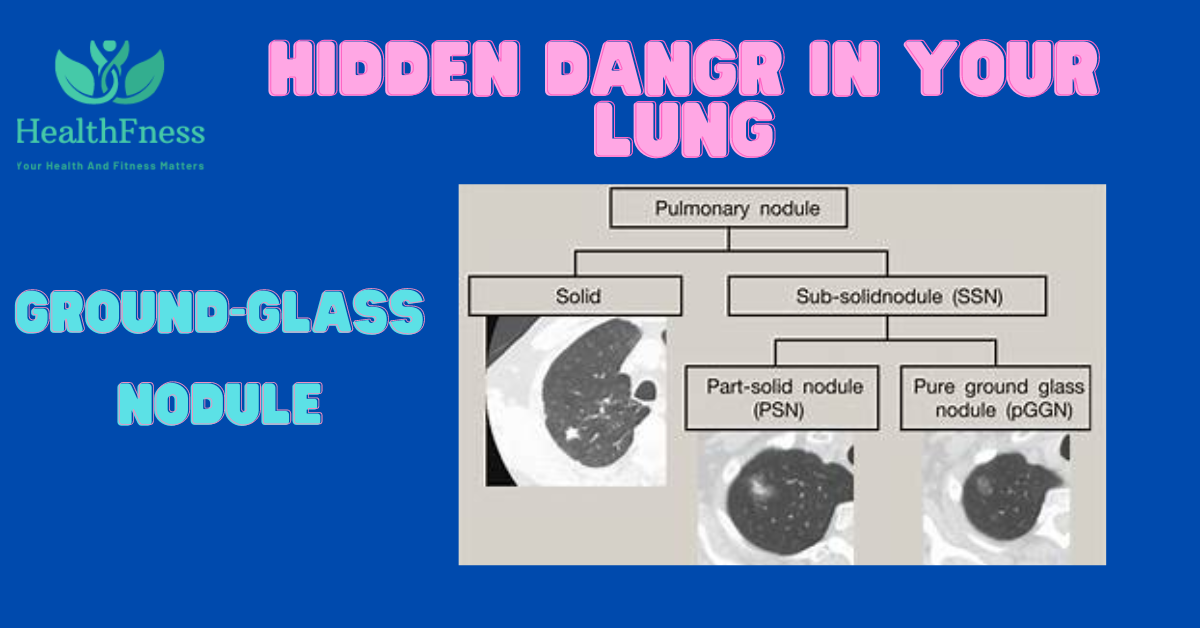
Ground glass nodules are abnormally dense regions of the lungs that on imaging assessments like computed tomography (CT) scans seem foggy or opaque. Identifying and managing these nodules are crucial because they’ll be symptoms of lung contamination and might become lung cancers sooner or later.
On imaging scans, those nodules may additionally show up as stable or semi-strong patches of opacity and may range in size, density, and form. While a few nodules may be benign and offer little risk, others can be symptoms of great lung conditions like most lung cancers.
It is essential to pick out ground glass nodules as quickly as possible due to the fact doing so allows short diagnosis and remedy. Healthcare practitioners can decide the high-quality route of movement for the patient by monitoring the development and evolution of those nodules at some stage in time.
Ground Glass Nodule ICD 10
The precise diagnosis and underlying cause of the ground glass nodule will determine the ICD-10 code for the nodule. For instance, if a lung infection caused the nodule, the classification would probably fall under J15 (Bacterial pneumonia, not otherwise categorized). The classification would probably come under C34 (Malignant neoplasm of bronchus and lung) if the nodule is determined to be a potentially malignant tumor.
Ground Glass Nodule In Lung
When a pitcher nodule is located in the lungs then it is known as a floor glass nodule within the lungs. They are called floor glass Ground glass, as utilized in scientific terminology, is a cloudy or hazy look seen on imaging assessments like computed tomography (CT) scans that denote a specific kind of lung disease.
Ground Glass Pulmonary Nodule
The word floor glass pulmonary nodule refers to a particular form of lung nodule determined. On imaging research, pulmonary nodules—small, rounded, or oval-shaped growths—can be visible. This indicates that the lung tissue in the nodule is in part packed with fluid, irritation, or aberrant cells whilst the nodules have a floor-glass appearance.
Broken Glass Nodules in Lungs
Multiple ground glass nodules that occur all over the lungs are known as damaged glass nodules. The underlying motives of those nodules vary in variety, along with inflammatory lung disease.
Causes Of Ground Glass Nodule
Following are some instances of lung situations that may result in ground glass nodules and their possible reasons:
Interstitial lung disorder (ILD)
The period ILD is used to describe a set of lung situations that bring about lung tissue irritation and scarring. Glass nodules can expand due to this scarring. ILD is thought to have several unknown reasons, some of which consist of autoimmune illnesses, exposure to pollutants inside the surroundings, and a few pills.
Pulmonary Fibrosis
Lung tissue will become thicker and scarier due to this form of ILD, making respiration tougher. The production of these nodules can also be stimulated by using scarring. Although the precise origin of pulmonary fibrosis is frequently unknown, it has been linked to genetic predispositions, drugs, and environmental pollutants.
Pneumonia
Pneumonia is a lung infection that could result in swelling and fluid accumulation or buildup of excess fluid, which can result in the development of floor glass nodules. Bacteria, viruses, and other organisms can all purpose pneumonia.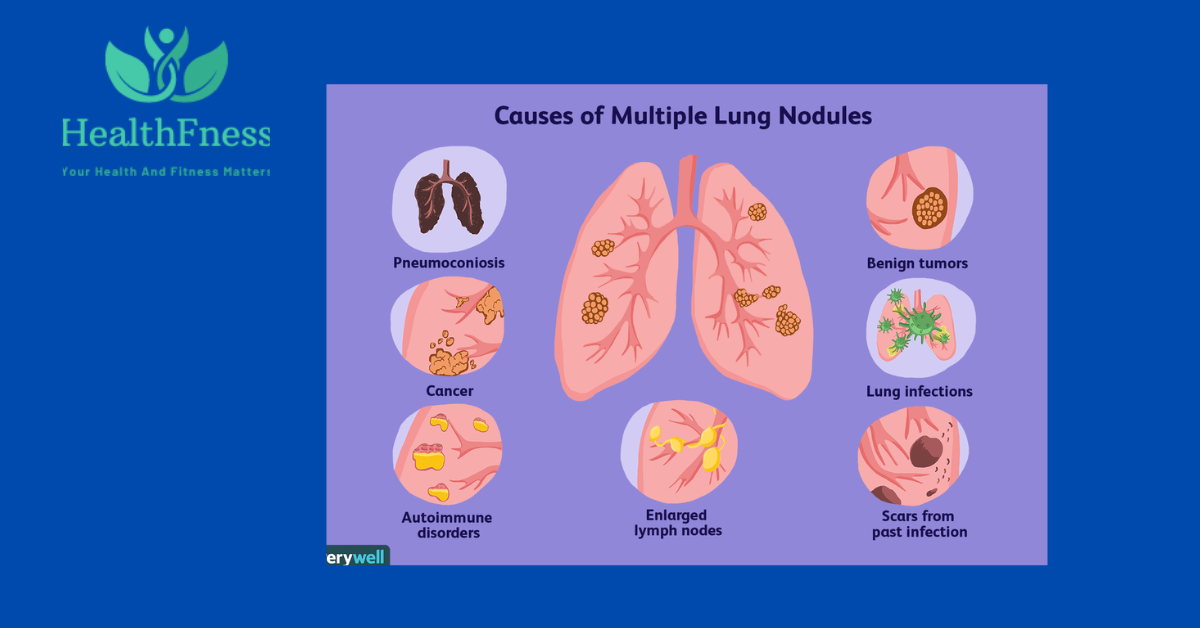
Tuberculosis
A bacterial contamination called tuberculosis usually affects the lungs. Ground glass nodules may also increase due to the contamination, which also can result in infection and scarring. When someone with tuberculosis coughs or sneezes, it spreads through the air and may be very contagious.
Lung cancer
These nodules may additionally arise as a result of lung cancer, which is a malignant tumor that can develop in the lung tissue. Smoking, exposure to environmental pollutants, and hereditary factors are frequently linked to lung cancers.
All of these causes can aid in developing ground glass nodules. Here are some more causes:
- Smoking: One of the primary hazard elements for floor glass nodules is smoking. It may damage the lungs and bring about nodules growing there.
- Chemical exposure: Exposure to asbestos, coal dirt, silica dirt, and other risky chemicals can affect the lungs and lift the chance of nodules developing.
- Age: People over the age of fifty are much more likely to have ground glass nodules.
- Family records: Ground glass nodules are much more likely to form in people with family records of lung illness or lung cancer.
- Gender: Ground glass nodules are extra, not unusual in girls than in guys.
NOTE: It is important to note that not all ground glass nodules are cancerous, and many are benign
Diagnosis Of Ground Glass Nodule
The following are some of the imaging checks usually used to detect those nodules:
Computed Tomography (CT) Scan
A CT test creates exceptional-grained go-sectional pics of the lungs with the use of X-rays and laptop technology. This imaging approach is especially beneficial for locating minute or undetectable ground glass nodules. Medical professionals can pick out the probable malignancy of nodules through the usage of statistics from CT scans on their size, form, and density.
Positron Emission Tomography (PET) Scan
A PET test creates photographs of the lungs with the usage of a small amount of radioactive material. To find and verify the metabolic hobby of floor glass nodules, this imaging technique is frequently used with a CT experiment. By tracking the metabolic activity of a nodule, PET scans can help in figuring out whether it is benign or cancerous.
Magnetic Resonance Imaging (MRI)
An MRI creates images of the lungs with the usage of radio waves and strong magnets. This imaging approach is regularly mixed with a CT test to offer additional information about the size, form, and area of this nodule and the doctor effortlessly perceives the hassle
Chest X-ray
A chest X-ray is a short imaging system that creates pics of the lungs with very little radiation. Although certain floor glass nodules can be seen on chest X-rays, they may be frequently no longer touchy sufficient to look smaller or extra sensitive nodules.
Ultrasonography
Ultrasonography creates pictures of the lungs using excessive-frequency sound waves. This imaging technique is regularly mixed with a CT test to feature the expertise about the location and dimensions of ground glass nodules. Because locating the location of the nodule is likewise very vital.
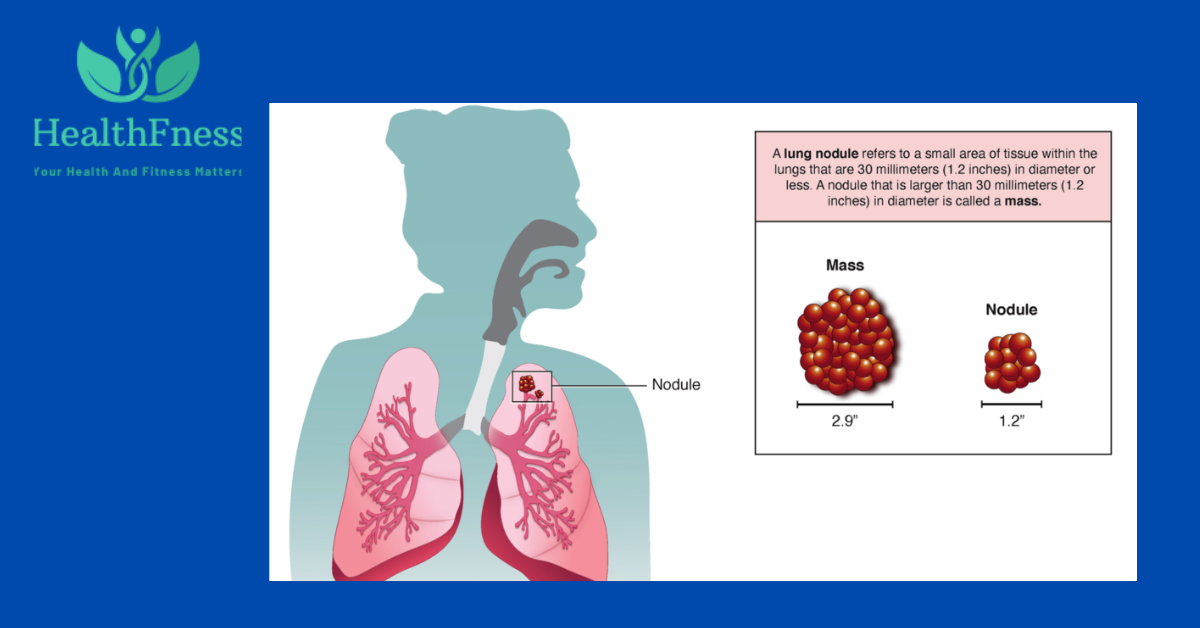
6mm Ground Glass Nodule In Lung
A 6mm ground glass nodule found within the lung is usually seen as tiny. However, the patient’s scientific records, threat elements, and the nodule’s imaging characteristics all play a role in how its miles are evaluated and managed. To song the nodule’s stability or increase through the years, a clinical practitioner could recommend more imaging examinations or observe-up scans.
8mm Ground Glass Nodule In Lung
A healthcare professional may additionally recommend a biopsy or surgical resection to gain a conclusive diagnosis depending on the unique traits and affected person elements. An 8mm floor glass nodule within the lung is barely larger than a 6mm nodule and can warrant closer assessment. Additional imaging research, such as positron emission tomography (PET) scans, may be cautioned to assess the nodule’s metabolic interest and determine the probability of malignancy.
How Radiologists Interpret Imaging Results
Radiologists are medical specialists who focus on analyzing imaging facts. Radiologists often look for several essential traits when deciphering imaging results for ground-glass nodules, together with:
- Size and location_Radiologists will measure the floor glass nodule’s length and record its place within the lungs. Important guidelines concerning the nodule’s underlying reason can be located inside the area.
- Shape and borders_Radiologists will search for abnormal or fuzzy borders, which can be a symptom of malignancy, as well as the shape of the ground glass nodule.
- Density_Radiologists will verify the density of the floor glass nodule considering this property can display statistics about the nodule’s possible malignancy. More thick nodules frequently have a higher most cancers chance.
- Growth Of nodule_Radiologists will screen the development of ground glass nodules over time when you consider that people who increase quickly can be malignant.
Radiologists will grade or assign a rating to the ground glass nodule based totally on these diagnostic tests and the way it is probably likely to be malignant. Ground glass nodules with smaller, extra regular borders and lower densities are frequently much less likely to be malignant or cancerous than people with larger, extra abnormal borders, and better densities.
Management Of Ground Glass Nodule
When a ground glass nodule is detected in the lungs, the management strategy is:
Management Strategy
A control technique known as watchful waiting; involves monitoring the nodule’s length and development over the years with ordinary imaging tests like CT scans. This approach is frequently carried out on nodules with easy borders, a small size (much less than 5mm), and a lower density. Avoiding unneeded surgical treatment or different intrusive strategies while still keeping a watch out for any signs of most cancers inside the nodule is the purpose of being watchful.
The affected person will usually agenda habitual follow-up visits with their doctor whilst cautiously ready to music the nodule’s development and any changes in its characteristics. The healthcare professional can also endorse additional checks or a biopsy if the nodule shows signs of growth or adjustments in its traits through the years to decide if it’s far cancerous.
Ground Glass Nodule Treatment
- Observation: Regular compliance with imaging tests can be used to display small, stable GGNs over time. The nodules are less likely to be malignant if they no longer increase or change in look over time.
- Biopsy: To obtain a tissue sample for added analysis, a biopsy may be advised if a GGN is suspicious or has famous growth-associated signs and symptoms. This aids in figuring out the benignity or malignancy of the nodule.
- Surgery may be important: to take away GGNs that are larger, growing, or have an excessive suspicion of most cancers. The lobectomy, additionally referred to as wedge resection, is a surgical procedure wherein the affected lung tissue containing the nodule is eliminated.
- Radiation Therapy: Radiation remedy is once in a while used to deal with situations, specifically in patients who aren’t applicants for surgery.
- Chemotherapy: As part of the remedy plan, chemotherapy may be cautioned if the GGN is cancerous and has spread outside of the lungs.
- Targeted remedy or immunotherapy: To extra exactly target most cancer cells or make the frame’s immune reaction in opposition to most cancers, medications can be prescribed for certain kinds of lung cancers.
Precautions Of Ground Glass Nodule After Treatment
There are some precautions one should take to recover fast:
- Follow up with healthcare providers
- Quit smoking
- Avoid exposure to harmful chemicals
- Maintain a healthy lifestyle
- Be aware of symptoms
- Follow recommended cancer screening guidelines
Reference
You would like to read this article:
Pulmonary Ground-Glass Nodules: Increase in Mass as an Early Indicator of Growth
The Conclusion of this study is: The examine realized that because of their heterogeneous nature and variable chance of malignancy, subsolid pulmonary nodules (SSNs) gift a diagnostic undertaking. It confused how vital it is to as it should be represented SSNs using imaging characteristics like length, density, and boom fee similarly to if needed, histopathological assessment.
The researchers pushed for a custom-designed approach to SSN management that took into consideration the precise traits of each affected person and struck a balance between the viable blessings of early detection and intervention in cases of malignancy and the risks of overdiagnosis and overtreatment. The take a look at additionally made clear the want for added investigation to improve danger assessment and control techniques for SSNs.
FAQS
A ground glass nodule (GGN) is what?
An area of elevated density inside the lungs that indicates up on imaging checks like CT scans as fuzzy or "ground glass" is referred to as a ground glass nodule. They are often located by twist of fate all through clinical imaging assessments and may be benign or malignant.
Why do floor glass nodules occur?
Lung cancer, scarring (fibrosis), infections, and irritation are among the reasons of GGNs. Finding the root reason often necessitates extra testing, like a biopsy or greater imaging scans.
Are all nodules fabricated from ground glass malignant?
No, now not each GGN develops cancer. In fact, quite a few GGNs are benign and won't need to be treated. However, it's critical to carefully examine GGNs because a number of them may additionally indicate early-stage lung most cancers or different serious conditions.
How are nodules of ground glass recognized?
CT scans and different imaging tests are typically used to locate GGNs. Additional imaging exams, which includes PET scans, and every so often a biopsy to eliminate a pattern of tissue for evaluation are part of the assessment method.
Which factors put someone at risk of getting floor glass nodules?
A history of lung illness, smoking, publicity to environmental pollution (inclusive of radon or asbestos), and unique genetic elements are threat elements for GGNs. GGNs, however, can also take place to people who have no acknowledged threat elements.
What path of movement is advised for floor glass nodules?
The size, shape, and growth fee of the nodules, in addition to the affected person's wellknown health and risk factors, all affect the path of remedy. Surgery, biopsies, and commentary are viable alternatives.
Are ground glass nodules always monitored, or do they require immediate treatment?
The approach to managing GGNs varies depending on the individual case. Small, stable nodules may be monitored over time with regular imaging tests, while larger or growing nodules or those with a high suspicion of cancer may require immediate intervention.
Conclusion
In conclusion, floor glass nodules may have more than a few underlying motives, ranging from infections to malignant growths. They are a huge finding in imaging studies. When comparing imaging consequences and deciding on the satisfactory route of movement, including surgical intervention or cautious readiness, radiologists are vital.
Patients with ground glass nodules need to consult with their health practitioner often to understand the ability dangers and recommended route of remedy, which may additionally contain ongoing statements, nutritional changes, or extra trying out. The diagnosis and recommended direction of treatment may be based in part on the size, form, and density of the nodule as well as the affected person’s scientific history.
Video Credits:

1 thought on “Ground Glass Nodule: The Hidden Danger in Your Lungs”