Corneal Edema is a condition in which the cornea, the clear outer layer of the eye, becomes swollen with fluid. This swelling can cause distortion or cloudiness of vision and may lead to permanent damage if left untreated.
This can affect people of all ages and genders men or women both, but it is more common in older adults and those with certain medical conditions, such as diabetes.
Early detection and treatment of corneal edema are crucial to prevent further damage to the cornea and maintain good vision.
Corneal Edema ICD 10👁️🗨️
The ICD-10 code H18.1 refers to corneal edema, which is the swelling of the cornea due to an accumulation of fluid. This code is used by healthcare professionals to identify and document cases of corneal edema in medical records and insurance claims.
This code can assist in the development of treatment plans and in obtaining insurance coverage for medical services related to the condition.
What Causes Corneal Edema
Corneal edema can have several underlying causes, including:
Endothelial Dysfunction
The cornea has a layer of cells called the endothelium that is responsible for pumping fluid out of the cornea and maintaining its clarity. Endothelial dysfunction or disturbance in the functioning of Endothelial, which can be caused by aging, certain medications, or underlying medical conditions, can impair the function of these cells, leading to this eye disorder.
Trauma Or Injury To The Eye
Physical trauma or injury to the eye can result in corneal edema. Examples include being struck in the eye or getting burned by chemicals.
Inflammatory Diseases
Certain inflammatory diseases, such as uveitis or iritis, can enlarge and inflame the cornea, resulting in this disease.
Post-surgical Complications
Corneal edema is a common complication following certain types of eye surgeries, such as cataract surgery or corneal transplant surgery.
Contact Lens wear
Prolonged or improper use of contact lenses can cause corneal edema due to the reduced oxygen supply to the cornea, irritation, or infection.
Symptoms Of Corneal Edema
If someone notices these symptoms seek medical attention as soon as possible. Corneal edema can cause a variety of symptoms, which may include:
Distorted or blurred vision_The corneal swelling can modify the curvature of the eye, which can result in distorted or impaired vision. The appearance of lines and objects may be wavy or crooked and a person feel confused.
Light sensitivity_An increase in the corneal fluid can result in photophobia and sensitivity to light. When exposed to bright light, such as sunshine or fluorescent lights, this may hurt or make you uncomfortable, and an itch in the eyes starts.
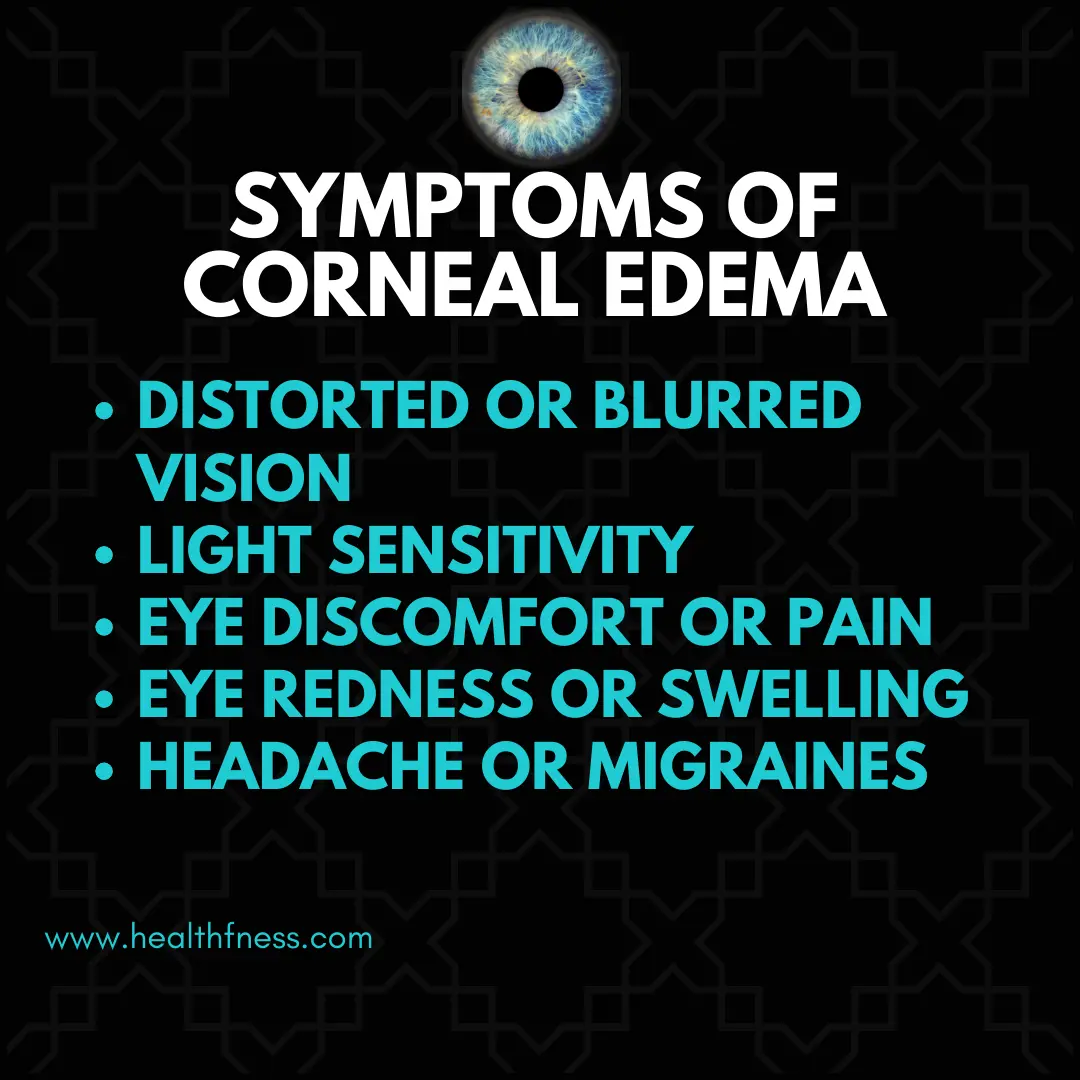
Eye discomfort or pain : This disorder may result in eye discomfort or pain. A dull soreness or a severe, stabbing pain may be experienced as a result.
Eye redness or swelling: Corneal edema occasionally results in redness and swelling around the eye. There may be ripping or discharge along with this.
Headache or migraines: Due to the pressure on the eyes and the heightened sensitivity to light, corneal edema can result in headaches or migraines.
Diagnosis of Corneal Edema
The following are some common methods used to diagnose corneal edema:
Physical Examination Of The Eye
A healthcare provider can undertake a physical examination of the eye to look for any outward indications of corneal edema, such as cloudiness or swelling of the cornea.
Visual AcuityTest
A visual acuity test is frequently used to gauge a person’s visual acuity at various ranges of distance. This examination can assist in detecting any vision alterations brought on by corneal edema.
Pachymetry
This non-invasive procedure measures the cornea’s thickness. This examination can assist identify the presence and potential severity of this disorder.
Specular Microscopy
This non-invasive imaging technique is used to look at the cells on the cornea’s inner surface. This examination might assist in identifying any cell damage that might be causing ocular edema.
Optical Coherence Tomography (OCT)
OCT is a non-invasive imaging procedure that uses light waves to produce an in-depth image of the cornea. This test can aid in identifying any alterations to the cornea’s structure brought on by corneal edema.
Corneal Edema Treatment
There are numerous treatment options available that help to cure this eye disease we will explain treatment options one by one.
Medications to reduce swelling and inflammation
Eye drops or ointments may be prescribed to reduce the swelling and inflammation in the cornea. These medications may include steroids or nonsteroidal anti-inflammatory drugs (NSAIDs) which aid in reducing swelling in the eyes and also decrease redness and itching in the eyes.
Corneal transplant surgery
A corneal transplant may be required in extreme circumstances to replace the diseased cornea with a healthy one. In this surgery, the damaged cornea is removed, and a donor cornea is used in its place.
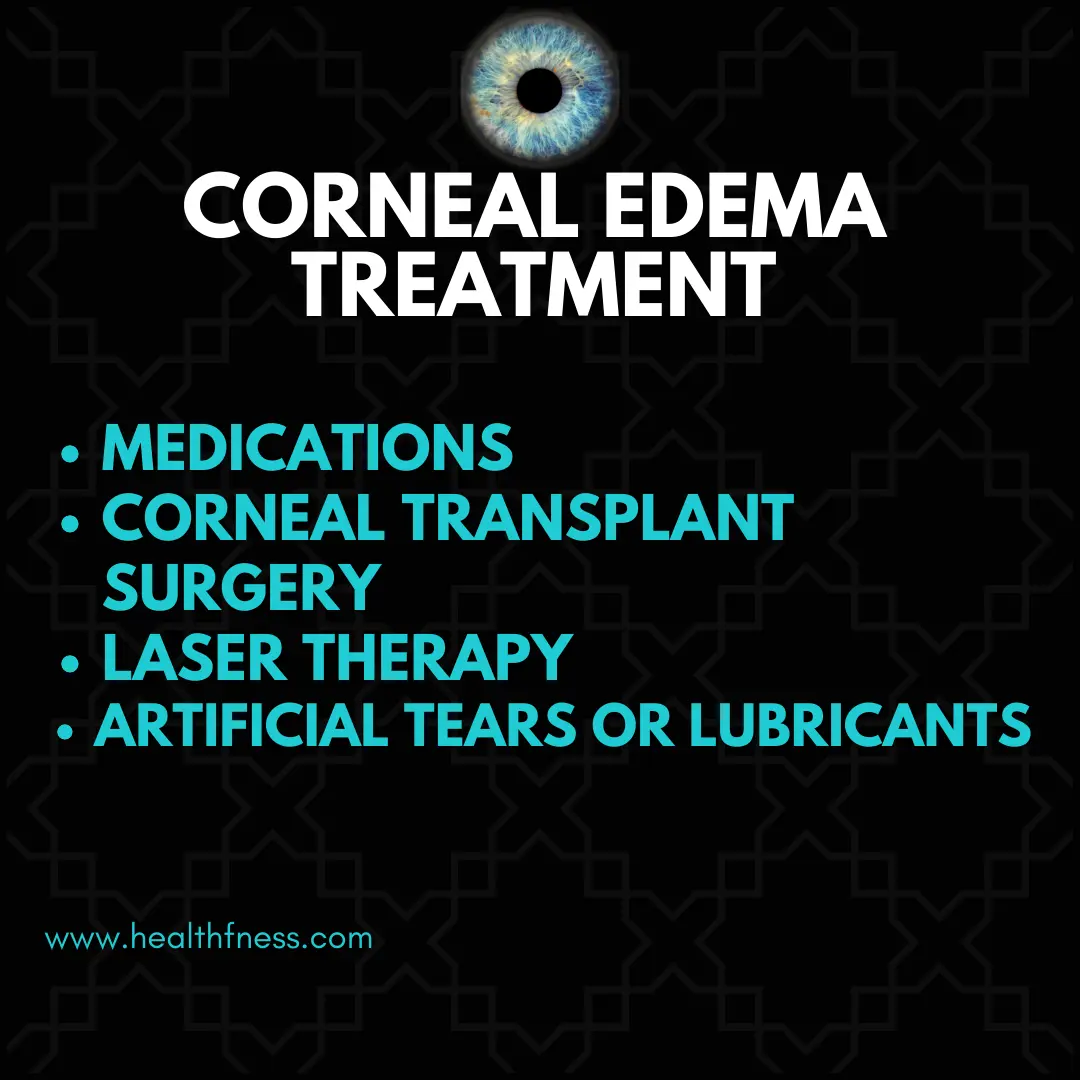
Laser therapy
When some disorders, such as Fuchs’ dystrophy, create corneal edema, laser therapy may be used to treat it. In this technique, the cornea is pierced with microscopic holes made by a laser, allowing extra fluid to drain.
Artificial tears or lubricants
These products are available over-the-counter and can be used to treat dryness and pain brought on by this eye disorder. These items can assist in maintaining the eye’s moisture and lowering the chance of additional injury. and also decrease eye dryness.
Complications And Prognosis of Corneal Edema
This can lead to several complications and affect a person’s quality of life. The following are some common complications and prognoses associated with corneal edema:
Potential for irreversible vision loss
Severe corneal edema can result in irreversible vision loss. If the underlying cause of the edema is not swiftly addressed or if the edema results in corneal scarring, this is more likely to happen.
Secondary infections
Because this eye disorder weakens the cornea, subsequent infections like bacterial or fungal infections might affect it more easily. These infections raise the risk of vision loss and can exacerbate corneal damage.
Prognosis with treatment
The prognosis for corneal edema is typically fair with proper diagnosis and treatment. In order to lessen swelling and inflammation, restore vision, and enhance the quality of life, patients may benefit from medications, laser therapy, and corneal transplant surgery.
Prevention Of Corneal Edema
While not all cases of this eye disorder are preventable, there are some measures that can be taken to reduce the risk of developing this condition. The following are some ways to prevent corneal edema:
- Regular eye exams
- Proper contact lens care and hygiene
- Management of underlying health conditions
- Avoidance of eye trauma or injury
FAQS:
What is the best treatment for corneal edema?
Treatment for corneal edema depends on the underlying cause. Options include hypertonic saline drops, steroids, endothelial keratoplasty, and surgical procedures such as Descemet's membrane endothelial keratoplasty (DMEK).
What causes corneal oedema?
Corneal edema can result from various factors like endothelial dysfunction, trauma, surgery complications, infections, glaucoma, and certain systemic conditions such as Fuchs' endothelial dystrophy or diabetes.
How long does corneal edema last?
The duration of corneal edema varies depending on its cause and severity. It can last from days to weeks or even months, requiring appropriate treatment for resolution.
Conclusion
Corneal Edema is a condition in which the outer layer of the eye becomes swollen and can cause distortion in vision. It can affect people of all ages and genders. The ICD 10 code for this disease is H18.1. Causes of corneal edema include endothelial dysfunction, trauma or injury to the eye, and wearing contact lenses for a long time. Symptoms can see in this disease like blur vision, light sensitivity, eye pain, and eye redness. Diagnosis can be done through visual activity tests, pachymetry, and OCT. The treatment options are available for this disease medication, eye drops, surgery, and laser therapy. One should take precautions like proper contact lens care and take care of hygiene and regular eyes checkup.
If you have any confusion or questions related to this topic do Let Us Know😊
Video Credits: