Low-dose naltrexone, or LDN, has rapidly gained attention as a versatile and promising treatment for a wide range of chronic health conditions. From autoimmune diseases like multiple sclerosis and Crohn’s disease to chronic pain syndromes such as fibromyalgia, patients and practitioners are exploring its potential. However, like any powerful medication, its effectiveness and safety hinge on understanding how it interacts with your body, other substances, and your unique health profile. Navigating this landscape can feel overwhelming, but being well-informed is the first step toward a successful treatment journey.
This comprehensive guide is designed to be your definitive resource on What to Avoid When Taking Low-Dose Naltrexone. We will delve into the critical interactions with opioids and alcohol, discuss caution with other medications and supplements, and outline special considerations for various medical conditions. By understanding these guidelines, you can work with your healthcare provider to harness the full potential of LDN while minimizing risks and ensuring your well-being.
Understanding Low-Dose Naltrexone (LDN)
Before we explore what to avoid, it’s crucial to understand what LDN is and how it differs from its standard-dose counterpart. This foundational knowledge will clarify why certain interactions are so dangerous.
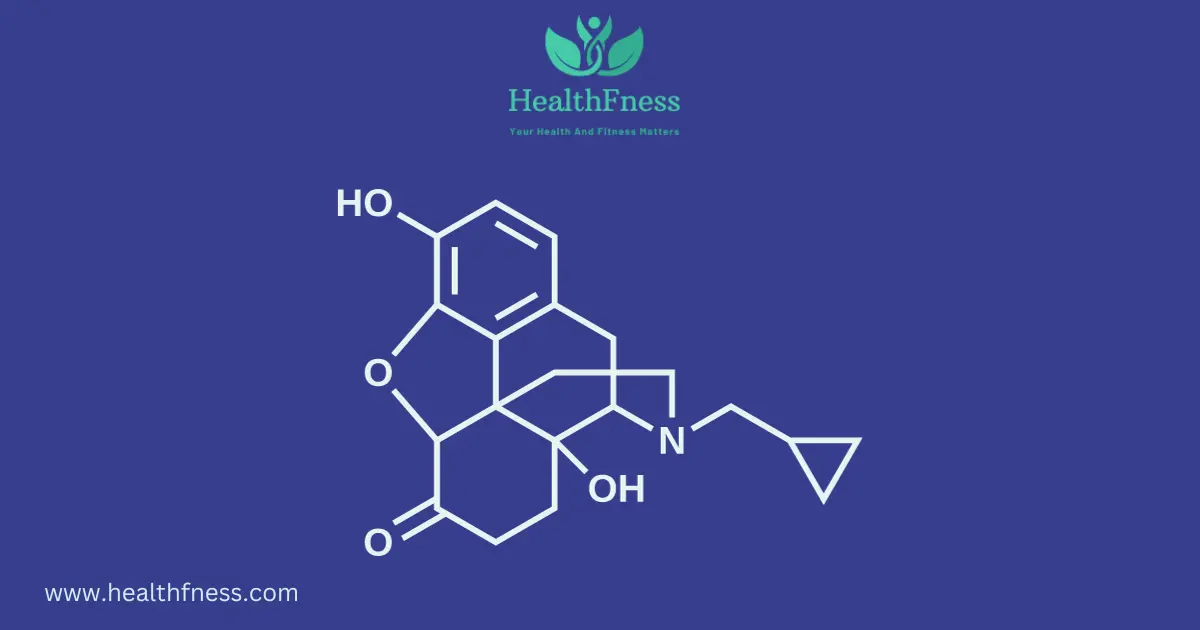
What is Naltrexone?
Naltrexone is a medication classified as an opioid antagonist. It was first approved by the U.S. Food and Drug Administration (FDA) in 1984. In its standard dosage, typically 50 to 100 milligrams per day, naltrexone is used primarily to treat Opioid Use Disorder (OUD) and Alcohol Use Disorder (AUD). It works by completely blocking opioid receptors in the brain. This action prevents the euphoric or “high” feelings associated with opioids and alcohol, which helps reduce cravings and supports recovery.
What Makes Low-Dose Naltrexone Different?
Low-dose naltrexone refers to the use of naltrexone in much smaller doses, typically ranging from 0.5 to 4.5 milligrams per day, though some protocols go up to 6 mg. This is considered an “off-label” use, meaning it’s prescribed for conditions other than those officially approved by the FDA. The mechanism of action at these low doses is believed to be fundamentally different and more nuanced.
Instead of a constant blockade of opioid receptors, LDN is thought to cause a brief, intermittent blockade. In response, the body is theorized to upregulate its production of endogenous opioids, namely endorphins and enkephalins. These are the body’s natural pain relievers and mood elevators. This temporary boost in “feel-good” chemicals is just one part of the story.
How Does LDN Work for Chronic Conditions?
The primary benefit of LDN for chronic conditions appears to stem from its powerful immunomodulating and anti-inflammatory effects. Research, including a notable 2014 review published in the Journal of Autoimmunity Reviews, suggests that LDN acts on non-opioid receptors, specifically Toll-like receptor 4 (TLR4), on immune cells in the central nervous system called microglia.
By blocking these receptors, LDN calms overactive microglia, reducing the production of inflammatory chemicals (cytokines) that drive chronic pain, fatigue, and tissue damage. This unique action is why LDN has shown promise for a wide array of inflammatory and autoimmune conditions, including:
- Fibromyalgia
- Multiple Sclerosis (MS)
- Crohn’s Disease and Ulcerative Colitis
- Chronic Fatigue Syndrome (ME/CFS)
- Hashimoto’s Thyroiditis
- Rheumatoid Arthritis
- Long COVID
The Absolute “Do Not Take” List: Critical Substances to Avoid
While LDN is generally well-tolerated, certain combinations are not just unhelpful, they are dangerous. The following substances must be strictly avoided to prevent severe adverse reactions.
1. Opioid Medications: The Most Critical Interaction
This is the most important rule of LDN therapy. Because naltrexone is an opioid antagonist, taking it with any opioid medication can trigger a severe and dangerous reaction known as precipitated withdrawal.
Why Opioids and LDN Don’t Mix: Understanding Precipitated Withdrawal
When someone is physically dependent on opioids, their body has adapted to the constant presence of these drugs. The opioid molecules are attached to receptors throughout the brain and nervous system. If naltrexone is introduced, it acts like a powerful magnet, forcefully kicking the opioid molecules off these receptors and blocking them. This sudden and complete reversal of opioid effects throws the body into an immediate and intense withdrawal state. Symptoms of precipitated withdrawal are far more severe and rapid in onset than natural withdrawal and can include:
- Severe nausea, vomiting, and diarrhea
- Intense muscle aches and cramping
- High fever, sweating, and chills
- Runny nose and watery eyes
- Extreme anxiety, agitation, and panic
- Rapid heart rate and high blood pressure
This condition can be a medical emergency and often requires hospitalization. It is absolutely critical to be completely free of opioids before starting LDN.
A Comprehensive List of Opioids to Avoid
You must avoid all forms of opioids, including prescription medications, illicit drugs, and even some surprisingly common over-the-counter products. This list is not exhaustive, so always consult your pharmacist or doctor if you are unsure.
- Prescription Pain Relievers: Codeine, Fentanyl, Hydrocodone (Vicodin, Norco), Hydromorphone (Dilaudid), Meperidine (Demerol), Methadone, Morphine, Oxycodone (OxyContin, Percocet), Oxymorphone, Tapentadol, Tramadol.
- Illicit Drugs: Heroin, illicitly manufactured fentanyl and its analogues.
- Opioid Use Disorder Treatments: Buprenorphine (Suboxone, Sublocade), Methadone.
- Over-the-Counter (OTC) & Other Medications:
- Loperamide (Imodium): This common anti-diarrhea medication is a weak opioid that acts primarily in the gut but can cause issues.
- Opioid-Containing Cough Syrups: Prescription cough medicines often contain codeine or hydrocodone.
The Crucial “Washout” Period
To safely begin LDN, you must have a “washout” period where you are completely opioid-free. The length of this period depends on the type of opioid used:
- Short-acting opioids (e.g., hydrocodone, oxycodone): A minimum of 7 to 10 days.
- Long-acting opioids (e.g., methadone, buprenorphine): A minimum of 10 to 14 days, and sometimes longer.
Your doctor may perform a urine drug screen or a naloxone challenge test to confirm that it is safe for you to start LDN.
2. Alcohol: A Risky Combination
While the interaction with alcohol is not as acutely dangerous as with opioids, it is still strongly advised to avoid or significantly limit alcohol consumption while on LDN for several key reasons.
Impact on Liver Health
Both naltrexone and alcohol are processed by the liver. In its standard, higher doses, naltrexone carries a warning for potential liver damage, although this risk is considered very low at the microdoses used in LDN therapy. However, combining it with regular or heavy alcohol use places an additional burden on the liver, potentially increasing the risk of liver inflammation or injury, especially in individuals with pre-existing liver conditions.
Masking Intoxication and Impaired Judgment
A significant danger of drinking on naltrexone is that it blocks the euphoric “buzz” or pleasurable effects of alcohol. A person might not feel drunk in the typical way. However, naltrexone does not prevent the other effects of alcohol, such as impaired judgment, poor coordination, slowed reflexes, and drowsiness. This creates a dangerous disconnect where an individual may consume far more alcohol than usual trying to achieve the desired feeling, leading to severe intoxication, accidents, or alcohol poisoning without realizing how impaired they are.
Diminished Treatment Efficacy
Alcohol is an inflammatory substance. For patients taking LDN to manage inflammatory or autoimmune conditions, consuming alcohol can counteract the anti-inflammatory benefits of the medication, potentially worsening symptoms and undermining the treatment’s effectiveness.
Proceed with Caution: Other Medications and Supplements
Beyond the absolute contraindications of opioids and alcohol, several other substances require careful consideration and a discussion with your healthcare provider.
3. Specific Prescription and Over-the-Counter (OTC) Drugs
Always review your complete medication list with your doctor and pharmacist before starting LDN.
- Immunosuppressants: Medications used to suppress the immune system, such as those taken after an organ transplant (e.g., cyclosporine, tacrolimus) or for severe autoimmune disease (e.g., methotrexate, biologics), may have conflicting actions with LDN. Since LDN works by modulating the immune system, combining it with a drug designed to suppress it can lead to unpredictable outcomes. This requires careful management by a specialist.
- Dextromethorphan (DXM): A common ingredient in many over-the-counter cough and cold remedies (e.g., Robitussin DM). Some research suggests DXM may interact with the same receptor pathways as LDN, potentially altering its effectiveness. While generally considered low risk, it’s wise to choose a cough medicine without it if possible.
4. Herbal Supplements and “Natural” Remedies
The term “natural” does not mean “safe.” Some herbal supplements can have powerful pharmacological effects and interact with medications like LDN.
- Kratom (Mitragyna speciosa): This herbal supplement has become popular for pain relief and managing opioid withdrawal. However, its primary active compounds act on opioid receptors. Taking kratom with LDN can trigger the same dangerous precipitated withdrawal symptoms as prescription opioids. Kratom must be strictly avoided.
- St. John’s Wort, Ginkgo Biloba, Echinacea: These and other supplements can affect liver enzymes that are responsible for metabolizing drugs. While no specific major interactions with LDN have been documented, altering its metabolism could theoretically change its effectiveness or side effect profile. Always inform your doctor about any supplements you are taking.
5. Recreational Drugs
Using recreational drugs while on LDN is incredibly risky. The primary danger lies with opioids like heroin or fentanyl, where the risk of precipitated withdrawal is high. Furthermore, because LDN blocks the euphoric effects, a user might take dangerously large doses to try and override the blockade, dramatically increasing the risk of a fatal overdose. The interactions with other substances like stimulants or hallucinogens are not well-studied and are unpredictable.
Important Considerations for Safe LDN Use
Effective LDN therapy involves more than just avoiding certain substances. It requires careful management in the context of your overall health.
Managing Special Medical Conditions
- Liver and Kidney Disease: Since naltrexone is metabolized by the liver and cleared by the kidneys, individuals with severe liver or kidney disease require close monitoring. Dosages may need to be adjusted, and regular lab work is essential to ensure safety.
- Autoimmune Disorders: While LDN is used for these conditions, it’s crucial to work with a doctor who understands its immunomodulating effects. Treatment should be coordinated with your specialist (e.g., rheumatologist, neurologist) to ensure it complements your existing therapy.
- Thyroid Conditions: LDN is frequently used by patients with Hashimoto’s thyroiditis, an autoimmune thyroid condition. Some patients report that as their immune system regulates, their need for thyroid hormone medication decreases. It is essential to monitor thyroid hormone levels (TSH, Free T4, Free T3) regularly after starting LDN to avoid becoming overmedicated.
- Pregnancy and Breastfeeding: Naltrexone is classified as FDA Pregnancy Category C, which means that risk to a fetus cannot be ruled out. While small amounts are known to pass into breast milk, harm has not been demonstrated. The decision to use LDN during pregnancy or breastfeeding must be made after a thorough risk-benefit discussion with your doctor.
Abruptly Stopping Low-Dose Naltrexone
LDN does not cause physical dependence or a traditional withdrawal syndrome. However, you should never stop taking it abruptly without consulting your doctor. Doing so can cause a sudden rebound of the symptoms for which you started the treatment (e.g., pain, fatigue, inflammation). If you need to discontinue LDN, your doctor may advise a gradual tapering of the dose.
Preparing for Surgery or Medical Emergencies
If you are taking LDN, you will not be able to receive opioid-based pain relief during and after a planned surgery or in an emergency. It is vital to:
- Inform your surgeon and anesthesiologist well in advance of any planned procedure. They will likely instruct you to stop LDN for several days to a week beforehand.
- Carry a medical alert card or wear a medical alert bracelet stating that you take naltrexone. This is crucial in case of an emergency where you are unable to communicate.
What Does the Latest Research Say?
The body of evidence supporting LDN continues to grow, with recent studies highlighting its potential and safety profile. For example, a 2023 systematic review published in Cureus analyzed existing studies on LDN for fibromyalgia. The authors concluded that LDN appears to be an effective, highly tolerable, and inexpensive treatment option for reducing fibromyalgia symptoms, reinforcing its place as a viable therapy. Further research is exploring LDN’s role in conditions like Long COVID, with preliminary findings suggesting its anti-inflammatory action on microglia may help alleviate neurological symptoms like brain fog and fatigue. As of 2024, multiple clinical trials are underway to further validate its efficacy for a variety of conditions, signaling a bright future for this repurposed medication.
Comparison Table: Low-Dose Naltrexone vs. Standard Dose Naltrexone
This table provides a clear, at-a-glance comparison of the two primary uses of naltrexone.
| Feature | Low-Dose Naltrexone (LDN) | Standard Dose Naltrexone |
|---|---|---|
| Typical Daily Dosage | 0.5 mg – 4.5 mg (sometimes up to 6 mg) | 50 mg – 100 mg |
| Primary Use | Off-label for autoimmune conditions, chronic pain, inflammation (e.g., Fibromyalgia, MS, Crohn’s) | Treatment of Alcohol Use Disorder (AUD) and Opioid Use Disorder (OUD) |
| FDA Approval Status | Not FDA-approved for these conditions (off-label use) | FDA-approved for AUD and OUD |
| Primary Mechanism of Action | Immunomodulation, anti-inflammatory effects (via microglia/TLR4), temporary endorphin increase | Complete and persistent blockade of opioid receptors to prevent euphoric effects |
| Common Side Effects | Generally mild and transient: vivid dreams, sleep disturbances, headache. Well-tolerated. | More pronounced: nausea, headache, dizziness, fatigue, anxiety, potential for liver enzyme elevation. |
Practical Tips for a Successful LDN Journey
To maximize your success with LDN, consider these best practices:
- Start Low, Go Slow: Most LDN protocols involve a slow titration, starting at a very low dose (e.g., 0.5 mg or 1.5 mg) and gradually increasing every week or two. This allows your body to adapt and minimizes potential side effects.
- Timing Your Dose: Traditionally, LDN is taken at bedtime, as the majority of endorphin production is thought to occur overnight. However, if you experience insomnia or vivid dreams, taking it in the morning is perfectly acceptable and equally effective for many.
- Keep a Symptom Journal: Track your symptoms, dosage, side effects, and overall well-being. This provides valuable data for you and your doctor to determine the optimal dose and assess progress.
- Be Patient: LDN is not a quick fix. While some people notice benefits within weeks, for many, it can take 3 to 6 months to experience the full therapeutic effects.
- Use a Reputable Compounding Pharmacy: Since LDN is not commercially available in low doses, it must be prepared by a compounding pharmacy. Ensure your pharmacy is experienced with LDN and does not use fillers that could inhibit absorption (like calcium carbonate) or slow-release binders.
Frequently Asked Questions About What to Avoid with LDN
Here are answers to some of the most common questions about LDN safety.
What happens if I accidentally drink a glass of wine on LDN?
For most people, a single, accidental drink is unlikely to cause a serious problem. However, you may not feel the usual pleasant effects from the alcohol, and you might still experience negative effects like poor coordination or a hangover. The primary concern is with regular or heavy drinking, which can stress the liver and undermine the medication’s benefits. It’s best to avoid alcohol altogether, but a minor, isolated slip-up is not usually a cause for panic. Discuss it with your doctor.
How long do I really have to be off opioids before starting LDN?
The 7-14 day rule is a firm medical guideline to prevent precipitated withdrawal. Do not try to shorten this window. The exact duration depends on the specific opioid, its half-life, and your level of physical dependence. Always follow your doctor’s specific instructions for your situation.
Can I take Tylenol (acetaminophen) or Advil (ibuprofen) with LDN?
Yes. Non-opioid pain relievers like acetaminophen and non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen do not interact with naltrexone. They are considered safe to use for pain or fever while taking LDN. However, always be mindful of the recommended daily limits for these medications, especially acetaminophen, to protect your liver.
What are the symptoms of taking too much low-dose naltrexone?
Taking a dose that is too high for you may not be dangerous, but it can negate the therapeutic effects and cause more side effects. Some people find that if they increase their dose too quickly or go too high, they experience a return of their symptoms (pain, fatigue) or increased side effects like headaches, anxiety, or irritability. This often means the dose should be lowered. The therapeutic “sweet spot” for LDN is highly individual.
Can I just stop taking LDN cold turkey?
While stopping LDN won’t cause a dangerous withdrawal, it’s not recommended. Abruptly ceasing the medication can lead to a significant rebound of the inflammatory symptoms it was suppressing. It’s always best to consult your healthcare provider, who will likely recommend a gradual taper to allow your body to readjust.
Does LDN interact with antidepressants (SSRIs)?
There are no known major negative interactions between LDN and common classes of antidepressants like SSRIs (e.g., Prozac, Zoloft) or SNRIs (e.g., Cymbalta, Effexor). Many people take these medications together safely. In fact, by reducing inflammation and boosting endorphins, LDN may even have a positive, synergistic effect on mood for some individuals.
Conclusion
Low-dose naltrexone offers a beacon of hope for millions struggling with chronic and often debilitating conditions. Its unique mechanism of action provides a powerful tool for modulating the immune system and reducing inflammation. However, its power demands respect and responsible use. The key to a safe and effective LDN experience is a clear understanding of what to avoid when taking low-dose naltrexone.
Remember the absolute rules: strictly avoid all opioids to prevent dangerous precipitated withdrawal, and abstain from alcohol to protect your liver and ensure the medication can work effectively. Beyond that, maintain open and honest communication with your healthcare provider about every medication, supplement, and health condition. By partnering with your doctor and adhering to these guidelines, you can safely navigate your treatment and unlock the remarkable potential of LDN on your journey toward better health.
References
- Younger, J., Parkitny, L., & McLain, D. (2014). The use of low-dose naltrexone (LDN) as a novel anti-inflammatory treatment for chronic pain. Clinical Rheumatology, 33(4), 451–459. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3962576/
- Patten, D. K., Schultz, B. G., & Berlau, D. J. (2018). The Safety and Efficacy of Low-Dose Naltrexone in the Management of Chronic Pain and Other Comorbid Symptoms: A Systematic Review. Journal of the American Pharmacists Association, 58(1), 91-99. https://pubmed.ncbi.nlm.nih.gov/29329933/
- Mayo Clinic. (2023). Naltrexone (Oral Route). https://www.mayoclinic.org/drugs-supplements/naltrexone-oral-route/precautions/drg-20068408
- Metyas, S., Chen, C., Yegiyants, S., Kechris, K., & Sayegh, S. (2023). Low-Dose Naltrexone in the Treatment of Fibromyalgia: A Systematic Review and Narrative Synthesis. Cureus, 15(5), e38446. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10276990/
- National Center for Biotechnology Information. (2024). Naltrexone. PubChem Compound Summary for CID 5360515. https://pubchem.ncbi.nlm.nih.gov/compound/Naltrexone

Dr. Mark Jenkins, MD - General Physician (California, USA)
Dr. Mark Jenkins is a board-certified general physician based in the United States, specializing in preventive medicine, nutrition, and lifestyle health. With years of clinical experience in primary care, he is dedicated to helping patients and readers alike make informed, science-based decisions about their well-being.
As a trusted medical reviewer and contributor to Healthfness.com, Dr. Jenkins ensures that all health content meets the highest standards of accuracy, safety, and evidence-based medicine. His expertise bridges modern medical science with practical, everyday wellness strategies, making complex topics approachable for all audiences.
Outside the clinic, Dr. Jenkins is passionate about living the healthy lifestyle he teaches. He enjoys hiking with his dog, experimenting with vegetarian cooking, and exploring the latest health research. He believes that small, consistent lifestyle changes lead to lasting health improvements, and he aims to inspire readers to take proactive steps toward a healthier, happier life.
Explore more of Dr. Jenkins’ evidence-based insights at Healthfness.com