What is Pancreatitis?
Pancreatitis is an endocrine organ located in the abdomen behind the stomach and it is the inflammation of the organ. Among the functions of the pancreas is the production of substances that enhance digestion in the small intestine and body’s regulation of sugar levels. Here we will discuss Acute Pancreatitis ICD-10 Code: K85.9 in detail.
You May Also Like To Read: Fatty Liver ICD 10: Life Expectancy With Fatty Liver Disease
Different codes of Pancreatitis ICD 10
Here are the different types of Pancreatitis ICD-10:
- Acute Pancreatitis ICD 10
- Chronic Pancreatitis ICD 10
- Gallstone Pancreatitis ICD 10
- necrotizing pancreatitis ICD10
- alcoholic pancreatitis ICD 10
- biliary pancreatitis ICD 10
- idiopathic pancreatitis ICD 10
Research work on Acute Pancreatitis ICD 10
Now we will go through different research on acute pancreatitis ICD-10. One study published in ScienceDirect examined the Risk Factors for Early Readmission After Acute Pancreatitis and the Importance of Timely Interventions. Another study on Pancreatitis ICD 10 is looked at by Taylor & Francis Online which is on Positive predictive values of ICD-10 codes to identify incident acute pancreatitis.
You May Also Like To Read: Lung Nodule ICD 10: Cracking The Code, Diagnosis, and Treatment
ICD 10 classifications for Pancreatitis Codes
Chronic Pancreatitis ICD 10
Chronic pancreatitis is a medical disorder in which the pancreas, a gland found behind the stomach that generates digestive enzymes and hormones such as insulin, is inflamed and damaged over time. The ICD-10 is the terminology used for the classification of conceptual systems of health care.
You May Also Like To Read: Lung Cancer ICD 10: Understanding The Code, Diagnosis, And Treatment
Gallstone Pancreatitis ICD 10
This type of pancreatitis arises when a gallstone becomes lodged in the bile duct, causing inflammation and damage to the pancreas. In ICD-10, the specific code for gallstone pancreatitis is K85.0.
Necrotizing Pancreatitis ICD10
This is a severe form of pancreatitis in which pancreatic tissue starts to fail. Necrotizing pancreatitis can be brought on by an array of reasons, including infection, injury, or pancreatic duct obstruction. In ICD-10, necrotizing pancreatitis is coded as K85.1.
Alcoholic Pancreatitis ICD 10
It’s a form of pancreatitis caused by long-term alcohol addiction. The process by which alcohol causes pancreatitis is uncertain or unknown, but it is believed to be connected to alcohol’s harmful effects on the pancreas. K85. 2 – Alcoholic pancreatitis ICD-10.
You May Also Like To Read: Diaphoresis ICD 10: What You Need To Know About Diaphoresis
Biliary Pancreatitis ICD 10
This is a type of pancreatitis that occurs when the bile duct becomes blocked, causing irritation and damage to the pancreas. A gallstone, tumor, or other obstruction might cause the blockage. In ICD-10, biliary pancreatitis is coded as K80.1.
Idiopathic Pancreatitis ICD 10
This is an instance of pancreatitis caused by unknown variables. In other words, there is no known cause of pancreas inflammation and damage. In ICD-10, the specific code for idiopathic pancreatitis is K85.9.
You May Also Like To Read: Pleural Effusion ICD 10: Exploring The Code And its Causes
Acute Pancreatitis ICD 10
Acute pancreatitis ICD-10 is an unexpected inflammation of the pancreas. The severity of the ailment can range from minor to life-threatening, necessitating hospitalization.
| Type of Pancreatitis | ICD-10 Code |
|---|---|
| Acute Pancreatitis | K85.9 |
| Chronic Pancreatitis | K86.1 |
| Gallstone Pancreatitis | K85.1 |
| Necrotizing Pancreatitis | K85.8 |
| Alcoholic Pancreatitis | K85.2 |
| Biliary Pancreatitis | K85.0 |
| Idiopathic Pancreatitis | K86.0 |
Causes and Risk Factors
There are numerous causes and risk factors associated with pancreatitis development.
Gallstones: The leading cause of acute pancreatitis is gallstones, contributing to approximately 35% of such incidences. There are stones in the gallbladder – This is gallstones: These are hard deposits that form in the gallbladder.
Alcohol Consumption: Another prominent cause of pancreatitis is excessive alcohol consumption, which accounts for around 25% of cases.
Medications: Medications that may cause pancreatitis include corticosteroids, diuretics, and some medications that are used to treat HIV.
Hypertriglyceridemia: Hypertriglyceridemia is a disease in which the blood contains great amounts of triglycerides, which are a type of fat.
Infections: Pancreatitis can be caused by infections such as mumps, CMV, and coxsackievirus. These infections can cause direct pancreatic injury.
Trauma: Pancreatitis can be caused by bodily trauma, such as a punch to the abdomen or a car accident. This can develop as a result of direct pancreatic irritation or disturbance of the pancreatic duct.
Inherited Factors: Some incidences of pancreatitis are positively associated with certain mutations such as changes in genes that are involved in regulating the function of the pancreas.
Other Risk Factors: Smoking, fatness, and some medical diseases, such as autoimmune pancreatitis and pancreatic cancer, are other risk factors for pancreatitis.
You May Also Like To Read: Vitamin D Deficiency ICD 10: Causes, Symptoms, and Treatment
Signs And Symptoms
The signs and symptoms of pancreatitis change according to the intensity of the disease, but some of the most prevalent symptoms are as follows:
Abdominal Pain
One of the most prevalent symptoms of pancreatitis is abdominal pain. The pain is usually in the upper abdomen and can be strong, persistent, and aggravated by food.
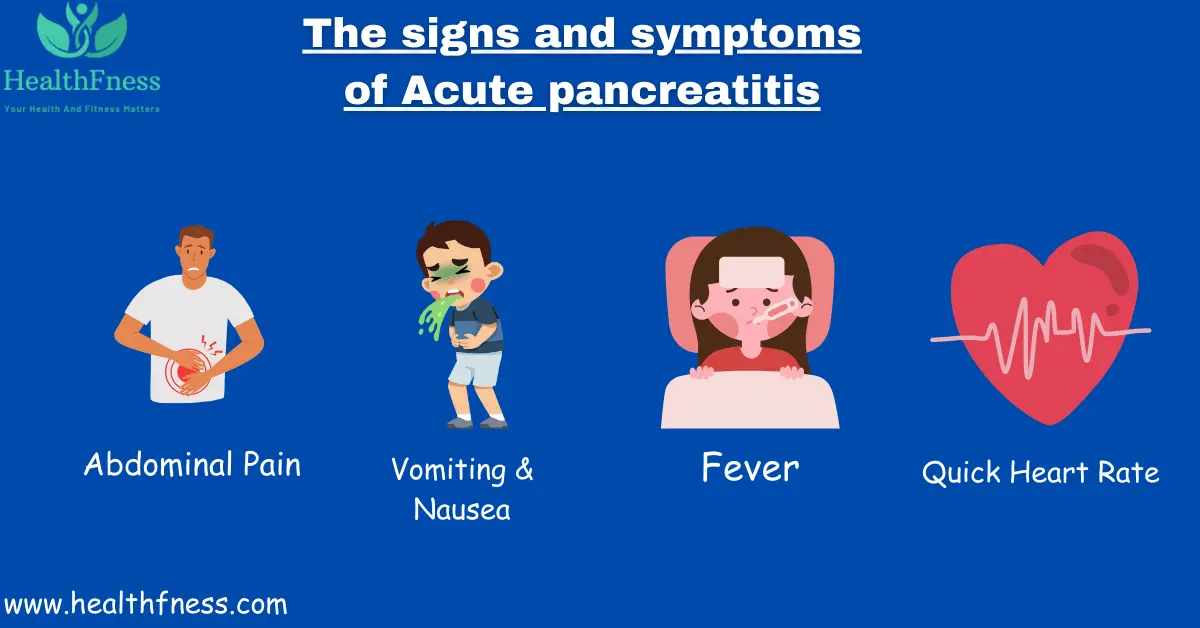
Vomiting and Nausea
Pancreatitis is characterized by nausea and vomiting, particularly during the acute phase of the ailment. Patients may feel queasy or have vomiting fits, which can be provoked by eating or drinking.
You May Also Like To Read: Iron Deficiency Anemia ICD 10: Unpacking Iron Deficiency Anemia
Fever
Fever is a common indicator of pancreatitis, particularly acute pancreatitis. The affected person may feel a high fever and sweat. The fever is usually caused by pancreatic inflammation, and it might be an indication of a more serious version of the disease.
Quick Heart Rate
A fast heart rate is a normal sign of pancreatitis, especially in acute pancreatitis ICD-10. High heart rate may also be indicative for other complications including sepsis which may develop in severe pancreatitis.
You May Also Like To Read: Cystic Fibrosis ICD 10: Unpacking Cystic Fibrosis and Cracking the Code ICD-10
Diagnosis of Acute Pancreatitis ICD-10
Pancreatitis is diagnosed through a series of:
Physical Examination and Medical History
A doctor will ask about a patient’s medical history, including any earlier experience of pancreatitis, alcohol usage, gallstone disease, and pancreatitis in the family.
Blood Tests
Tests using blood samples may also be used to diagnose pancreatitis. It is, however, noteworthy that amylase and lipase are the two most commonly elevated pancreatic enzymes in patients suffering from pancreatitis.
Imaging Tests
Imaging tests are used to visualize the pancreas and surrounding organs. Common imaging tests used in the diagnosis of pancreatitis include ultrasound, CT scan, and MRI.
Other Diagnostic Procedures
Further diagnostic tests may be required in some circumstances to identify pancreatitis. Stool tests to look for fat in the feces, which might suggest poor digestion.
You May Also Like To Read: Prediabetes ICD 10: Types, Causes, And Treatment
Treatment of Acute Pancreatitis ICD-10
Acute pancreatitis is a serious condition that requires prompt medical attention.
Hospitalization and Supportive Care
The majority of treatment depends on the severity of patients requiring hospitalization. Patients in extreme situations may need to be hospitalized in the ICU (ICU). Here are some instances of supportive care:
NPO status: Patients are placed on nothing-by-mouth (NPO) status, which means they cannot eat or drink anything until the inflammation subsides. This gives the pancreas time to relax and repair.
Intravenous fluids: Fluids are administered to patients via an IV to prevent dehydration and maintain electrolyte balance.
Oxygen therapy: Supplemental oxygen is provided to patients who are in respiratory distress.
Monitoring vital signs: Vital indicators, such as blood pressure, heart rate, and breathing rate, are carefully monitored.
Pain Management
Severe abdominal pain can be produced by acute pancreatitis. undefined:
Medications: Analgesics like acetaminophen, and ibuprofen may be administered; or opioids may be used.
Nerve blocks: Nerve blocks may be used to inhibit pain impulses in some circumstances.
You May Also Like To Read: Understanding Hyperparathyroidism ICD 10: Symptoms, Causes, and Treatments
Nutritional Assistance
Many patients have chronic pancreatitis that causes an aversion to food due to nausea, vomiting, and abdominal pain. Nutritional assistance includes:
Enteral feeding: Feeding through a tube inserted through the nose and into the stomach or small intestine is known as enteral feeding.
Total parenteral nutrition (TPN): Feeding through an IV.
Therapy of the Root Causes
There will be a need to identify the cause of the condition to prevent future acute pancreatitis. undefined
Surgery: Surgery may be required to remove gallstones or damaged pancreatic tissue.
Medications: Medicines may be recommended to decrease cholesterol levels or to treat underlying medical issues.
You May Also Like To Read: Understanding of Menopause ICD 10: How ICD-10 Helps with Diagnosis and Treatment
Prevention
While there is no definite method to avoid pancreatitis, there are things you may do to lower your chances of getting it. The following are some of the methods in which one should avoid pancreatitis.
Lifestyle Changes
Prevent Excessive Alcohol Consumption
Excessive alcohol use is a key risk factor for pancreatitis. Persistent alcohol intake can cause pancreatic inflammation and raise the chance of developing pancreatitis.
Keep a Healthy Diet
Exercise
Frequent exercise will help you maintain a healthy weight and lower your risk of obesity, which is a risk factor for pancreatitis.
Stop smoking
Smoking is not only bad for your lungs, but it also raises your chance of pancreatitis. Stopping smoking can lower your chances of developing pancreatitis.
You May Also Like To Read: Chronic Pancreatitis ICD 10: Types, Causes, and Prevention
Life Expectancy After Acute Pancreatitis
The severity of the ailment, the underlying reasons, the patient’s general health, and the efficacy of treatment all affect how long someone will live following an incident of acute pancreatitis. The long-term outlook is often favourable in mild cases that are rapidly treated and resolved, and people can anticipate a typical life expectancy.
FAQS
What is the most common sign of acute pancreatitis?
Abdominal pain that is severe and persistent is a symptom of acute pancreatitis.A sharp pain may be felt on the back or chest which starts from the upper abdomen. The pain can also increase after meals and beverages and be chronic, burning, or piercing discomfort. Other symptoms associated with acute pancreatitis include nausea, vomiting, and fever, rapid pulse, and a distended or pain abdomen.
What does ICD-10 code K85 mean?
Acute pancreatitis is A form of the disease where the pancreas in most cases becomes inflamed and leads to severe abdominal pain and vomiting. This code is useful to group and record acute pancreatitis cases in the medical system as well as used in insurance processes. However, it should be noted that each type of acute pancreatitis is associated with its own ICD-10 code – alcohol-induced, gallstones, etc.
What is the History of pancreatitis ICD-10?
In 1992, the ICD-10 system's 10th version included the first appearance of the pancreatitis code. Acute pancreatitis received the number K85, while chronic pancreatitis received the code K86.1. Pancreatitis was given its own set of codes to allow for better tracking and care of this ailment, which can be fatal if left untreated.
What are the symptoms of Acute pancreatitis?
A sudden, severe stomach pain that frequently radiates to the back is the typical initial symptom of acute pancreatitis. Along with this pain, nausea, vomiting, and a painful abdomen may also occur. Fever, an accelerated heartbeat, and a reduction in blood pressure are possible symptoms for patients. Additionally, there may be signs like bloating, indigestion, and appetite loss.
What is the best treatment for acute pancreatitis?
Supportive care, pain control, and addressing the underlying cause are the main components of the treatment for acute pancreatitis. Treatment for mild cases frequently includes fasting to give the pancreas a break, intravenous fluids to avoid dehydration, and medicines for pain relief. Hospitalisation may be necessary for severe instances, at which time patients get intensive observation and food support via feeding tubes.
Conclusion
Chronic pancreatitis is a medical disorder that causes long-term inflammation and damage to the pancreas, a gland located behind the stomach that produces digestive enzymes and hormones such as insulin. The illness can cause a variety of symptoms such as abdominal pain, weight loss, nausea, and vomiting.
Video Credits:

Dr. Mark Jenkins, MD - General Physician (California, USA)
Dr. Mark Jenkins is a board-certified general physician based in the United States, specializing in preventive medicine, nutrition, and lifestyle health. With years of clinical experience in primary care, he is dedicated to helping patients and readers alike make informed, science-based decisions about their well-being.
As a trusted medical reviewer and contributor to Healthfness.com, Dr. Jenkins ensures that all health content meets the highest standards of accuracy, safety, and evidence-based medicine. His expertise bridges modern medical science with practical, everyday wellness strategies, making complex topics approachable for all audiences.
Outside the clinic, Dr. Jenkins is passionate about living the healthy lifestyle he teaches. He enjoys hiking with his dog, experimenting with vegetarian cooking, and exploring the latest health research. He believes that small, consistent lifestyle changes lead to lasting health improvements, and he aims to inspire readers to take proactive steps toward a healthier, happier life.
Explore more of Dr. Jenkins’ evidence-based insights at Healthfness.com