Do you wake up feeling more exhausted than when you went to bed? Does your partner complain about your loud, disruptive snoring? While many factors can contribute to poor sleep, one surprising culprit might be hiding in plain sight: the alignment of your jaw. It may sound far-fetched, but a growing body of scientific evidence reveals a powerful connection between your dental structure, specifically an overbite, and a serious sleep disorder known as obstructive sleep apnea (OSA). In fact, many people wonder, can an overbite cause sleep apnea? The answer is yes, it can play a major role in restricting airflow during sleep, leading to breathing interruptions and restless nights.
Many people dismiss an overbite as a simple cosmetic issue, but its implications can run much deeper, directly impacting your airway and your ability to breathe properly during sleep. This comprehensive guide will explore the intricate relationship between an overbite and sleep apnea, delving into the underlying causes, associated health risks, and the modern treatment options that can restore your sleep and safeguard your long-term health. If you’ve ever wondered whether your bite is to blame for your restless nights, you’re in the right place.
What Exactly is an Overbite?
Before we explore the link to sleep apnea, it’s essential to understand what an overbite is. In dentistry, the term for a misaligned bite is malocclusion. An overbite, technically known as a Class II malocclusion, is a specific type where the upper front teeth significantly overlap the lower front teeth.
A small amount of overlap (around 1-2 millimeters) is perfectly normal and even ideal for proper chewing function. However, when the overlap is excessive, it’s referred to as a “deep bite” or a significant overbite. This condition often occurs because the lower jaw, or mandible, is set back relative to the upper jaw (a condition called retrognathia). This backward positioning of the jaw is the crucial element that connects an overbite to breathing problems.
Common Causes of an Overbite:
- Genetics: The size and shape of your jaw are largely inherited. If your parents had an overbite, you are more likely to have one as well.
- Childhood Habits: Prolonged habits during developmental years can influence jaw growth. These include thumb-sucking, extended pacifier use, or tongue-thrusting (pushing the tongue against the front teeth when swallowing).
- Missing or Crowded Teeth: Irregularities in tooth eruption or spacing can also contribute to the development of a misaligned bite over time.
Understanding Sleep Apnea: More Than Just Snoring
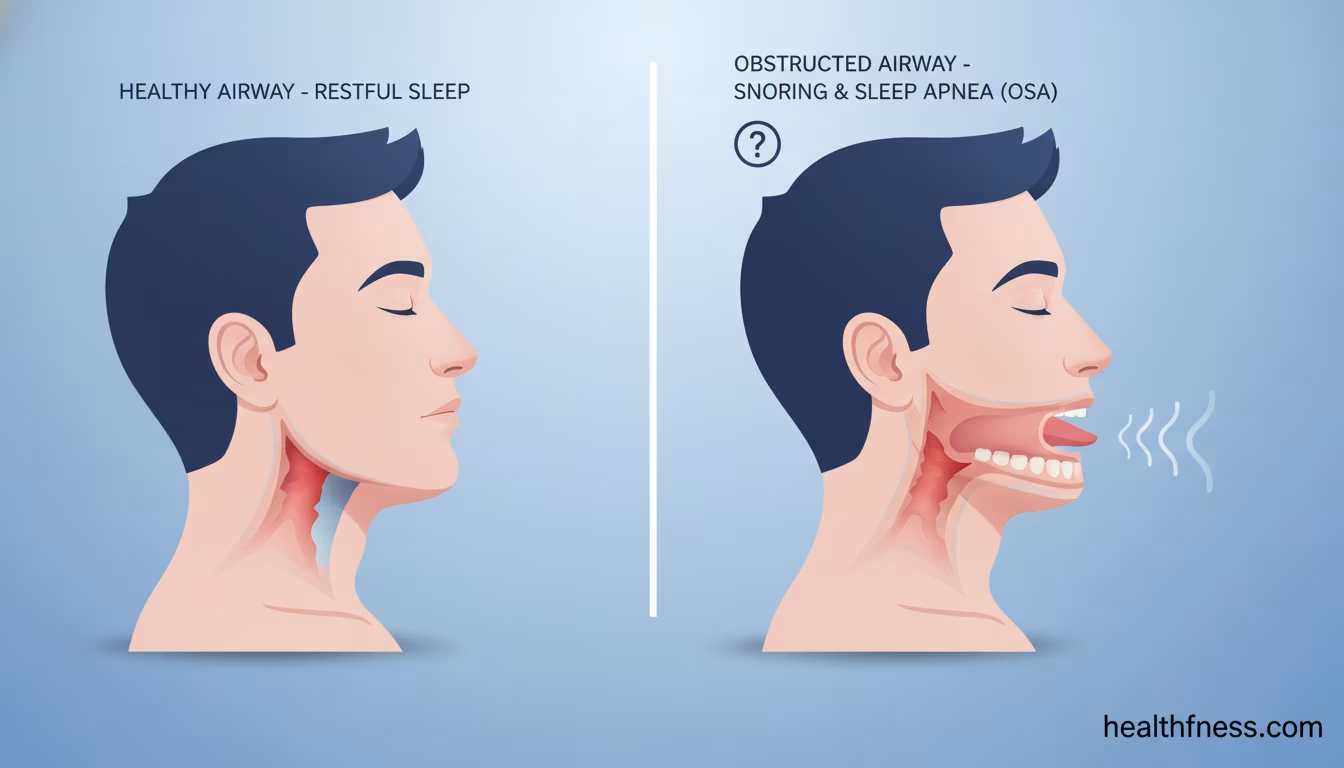
Sleep apnea is a potentially serious sleep disorder where breathing repeatedly stops and starts throughout the night. While loud snoring is a hallmark symptom, the condition is far more dangerous than that. These pauses in breathing, called “apneas,” can last for ten seconds or longer and occur dozens or even hundreds of time per night.
There are three main types of sleep apnea:
- Obstructive Sleep Apnea (OSA): This is by far the most common form and the one directly linked to overbites. It happens when the muscles in the back of the throat relax excessively during sleep, allowing soft tissues (like the tongue and soft palate) to collapse and physically block the airway.
- Central Sleep Apnea (CSA): This is a less common neurological issue where the brain fails to send the proper signals to the muscles that control breathing. The airway is not blocked, but the body makes no effort to breathe.
- Complex (or Mixed) Sleep Apnea Syndrome: This is a combination of both OSA and CSA.
When an apnea occurs in OSA, your brain senses the drop in oxygen and surge in carbon dioxide. It sends a panic signal to momentarily wake you up just enough to reopen your airway, often with a loud gasp, snort, or body jerk. Because these awakenings are so brief, most people with sleep apnea have no memory of them, yet their sleep is profoundly fragmented, preventing them from reaching the deep, restorative stages of sleep.
How Can an Overbite Cause Sleep Apnea? The Anatomical Connection
The link between an overbite and OSA is not coincidental; it’s a direct result of anatomy and physics. The position of your jaw dictates the amount of space available in your upper airway. A significant overbite, especially one caused by a recessed lower jaw, creates a cascade of problems that compromise this critical space.
The Chain Reaction: From Jaw Position to Airway Collapse
Imagine your airway as a flexible tube running down your throat. The stability of this tube depends on the structures surrounding it. Here’s how an overbite disrupts this stability:
- Recessed Lower Jaw: In a classic overbite scenario, the lower jaw is positioned too far back.
- Backward Tongue Placement: The tongue is a large muscle, and its base is attached to the inside of the lower jaw. When the jaw is recessed, the entire tongue is also forced to sit further back in the mouth.
- Narrowed Airway: This backward displacement of the tongue physically encroaches on the pharyngeal airway, the space behind the tongue. Even when you are awake, this space is already smaller than it should be.
- The Sleep Factor: When you fall asleep, all the muscles in your body relax, including your tongue and throat muscles. In an already narrowed airway, this relaxation is the final straw. The tongue falls back even further, acting like a cork that completely or partially seals off the airway.
- Breathing Stops: Airflow is obstructed, oxygen levels in your blood plummet, and an apneic event occurs. Your brain then forces a micro-awakening to restore muscle tone and reopen the airway, and the cycle repeats all night long.
A study published in the Cranio: The Journal of Craniomandibular & Sleep Practice in 2019 specifically found that skeletal characteristics, such as a recessed mandible (common in overbites), are significant predisposing factors for the development of obstructive sleep apnea.
Overbite, TMJ, and Sleep Apnea: A Troubling Trio
An overbite can also contribute to Temporomandibular Joint Disorder (TMD), a condition causing pain and dysfunction in the jaw joint and the muscles that control jaw movement. The misalignment from an overbite puts chronic strain on the TMJ. This can lead to inflammation, pain, clicking or popping sounds, and headaches. Furthermore, individuals with TMD often grind their teeth at night (bruxism), another sleep disorder that can be exacerbated by the body’s struggle to keep the airway open. This creates a vicious cycle where the poor bite structure contributes to both sleep apnea and TMJ, and the symptoms of each can worsen the other.
Why Treating an Overbite for Sleep Apnea Matters
Addressing the root structural problem, the overbite, is not just about achieving a straighter smile or quieting snoring. It’s a critical step toward improving your overall health and quality of life. The benefits of diagnosing and treating overbite-related sleep apnea are profound and far-reaching.
Beyond a Good Night’s Sleep: The Systemic Health Benefits
When you effectively treat sleep apnea, you allow your body to get the restorative sleep it needs to function properly. This leads to:
- Improved Cardiovascular Health: Untreated sleep apnea puts immense strain on the heart. Each apneic event causes a spike in blood pressure and heart rate. A 2021 report from the American Heart Association emphasizes that treating sleep apnea can significantly lower blood pressure and reduce the risk of heart attack, stroke, and atrial fibrillation.
- Enhanced Cognitive Function: Chronic sleep deprivation impairs memory, concentration, and executive function. Restoring quality sleep can lead to sharper thinking, better focus at work or school, and improved memory recall.
- Stable Mood and Mental Well-being: The link between poor sleep and mood disorders like depression and anxiety is well-established. Treating sleep apnea can lead to a more stable mood and an overall better sense of well-being.
- Reduced Daytime Fatigue: One of the most immediate benefits is the elimination of excessive daytime sleepiness. This means more energy for daily activities, reduced reliance on caffeine, and a lower risk of falling asleep while driving or operating machinery.
Aesthetic and Functional Dental Benefits
Beyond the systemic health improvements, correcting the overbite itself yields significant oral health benefits:
- Improved Facial Aesthetics: Correcting a recessed lower jaw can improve your facial profile, creating a more balanced and harmonious appearance.
- Better Chewing Efficiency: A properly aligned bite allows you to chew food more effectively, which can aid in digestion.
- Reduced Tooth Wear: A deep overbite can cause the lower front teeth to strike the roof of the mouth or the back of the upper teeth, leading to accelerated and abnormal wear of your enamel.
- Alleviation of TMJ Symptoms: By moving the jaw into a more natural and stable position, orthodontic treatment can relieve the strain on the jaw joints, reducing pain, headaches, and other TMD symptoms.
The Dangers of Untreated Overbite-Related Sleep Apnea
Ignoring the symptoms of sleep apnea, whether caused by an overbite or other factors, can have devastating consequences for your health. The chronic cycle of oxygen deprivation and sleep fragmentation acts as a major stressor on nearly every system in your body.
Systemic Health Complications
- High Blood Pressure (Hypertension): The recurrent drops in blood oxygen levels trigger the release of stress hormones, which constrict blood vessels and raise blood pressure over time. OSA is a recognized independent risk factor for hypertension.
- Heart Disease: The constant stress on the cardiovascular system increases the risk of heart attacks, congestive heart failure, and irregular heartbeats (arrhythmias).
- Stroke: According to the American Stroke Association, sleep apnea significantly increases the risk of stroke, partly due to its effects on blood pressure and oxygen supply to the brain.
- Type 2 Diabetes: Sleep apnea is strongly linked to insulin resistance. A landmark study from the Sleep Heart Health Study, with ongoing analysis into the 2020s, has consistently shown that sleep-disordered breathing impairs glucose metabolism, increasing the likelihood of developing type 2 diabetes.
- Cognitive Decline: Emerging research suggests that long-term, untreated OSA may be a risk factor for cognitive impairment and even dementia later in life due to chronic oxygen deprivation to the brain.
Daily Life Impairment
- Accidents: The National Highway Traffic Safety Administration (NHTSA) estimates that drowsy driving, a major consequence of sleep apnea, is responsible for thousands of crashes, injuries, and fatalities each year.
- Decreased Quality of Life: Constant fatigue, irritability, and mood swings can strain personal and professional relationships, leading to a diminished quality of life.
What Does the Research Say? Evidence Linking Overbites and Sleep Apnea
The connection between jaw structure and sleep apnea is not just a theory; it is supported by decades of clinical research using advanced imaging and diagnostic tools. Here are some key findings from recent studies that solidify this link:
- A foundational study in the American Journal of Orthodontics and Dentofacial Orthopedics from 2015 used 3D imaging to demonstrate that patients with Class II malocclusion (overbites) had a significantly narrower and longer upper airway compared to those with normal bites, predisposing them to airway collapse during sleep.
- A systematic review published in the Journal of Clinical Sleep Medicine in 2020 analyzed multiple studies and concluded that orthodontic treatments aimed at advancing the mandible (lower jaw) are an effective therapy for reducing the severity of OSA, particularly in mild to moderate cases. This directly supports the idea that correcting the structural issue of an overbite can treat the resulting breathing problem.
- Research focusing on pediatric patients, such as a 2022 study in the journal Sleep and Breathing, has shown that early orthodontic intervention in children with recessed jaws and narrow palates can guide facial growth in a way that enlarges the airway, potentially preventing the development of OSA in adulthood. This highlights the importance of early evaluation and treatment.
These studies, among many others, confirm that an overbite is more than a cosmetic concern, it is a significant anatomical risk factor for obstructive sleep apnea. This evidence-based understanding has paved the way for more integrated treatment approaches involving both sleep medicine and orthodontics.
Comparing Treatment Options for Overbite-Related Sleep Apnea
If you’re diagnosed with sleep apnea and have a significant overbite, you have several effective treatment pathways. The best option depends on the severity of your sleep apnea, the degree of your overbite, your personal preferences, and a consultation with your healthcare team. Here’s a comparison of the most common approaches:
| Treatment | How It Works | Best For | Pros | Cons |
|---|---|---|---|---|
| CPAP (Continuous Positive Airway Pressure) | A machine delivers a steady stream of pressurized air through a mask, acting as an “air splint” to keep the airway from collapsing. | Moderate to severe sleep apnea. It’s the gold standard for treatment. | Highly effective; Immediate relief; Non-invasive. | Bulky and noisy; Can be uncomfortable; Requires nightly use; Does not fix the underlying overbite. |
| Oral Appliance Therapy (MADs) | A custom-fitted mouthguard (Mandibular Advancement Device) worn at night that gently pushes the lower jaw forward, opening the airway. | Mild to moderate sleep apnea; Patients who cannot tolerate CPAP. | Portable and silent; Comfortable for most; Easy to use. | Less effective for severe cases; Can cause jaw soreness or bite changes; Does not permanently correct the overbite. |
| Orthodontic Treatment (Braces/Invisalign) | Gradually moves the teeth and can influence jaw position to permanently correct the overbite, thereby enlarging the airway space. | Patients whose overbite is a primary cause of their mild to moderate sleep apnea. Often used in conjunction with other therapies. | Permanent solution to the structural problem; Improves dental health and aesthetics; No nightly device needed after treatment. | Longer treatment time (1-3 years); Can be costly; May not be sufficient for severe OSA on its own. |
| Corrective Jaw Surgery (Orthognathic Surgery) | A surgical procedure to physically reposition the upper and/or lower jaw into a more favorable alignment, drastically opening the airway. | Severe overbites and severe sleep apnea where other treatments have failed. | Potentially curative for both the overbite and sleep apnea; Dramatic improvement in function and aesthetics. | Invasive procedure with significant recovery time; Carries surgical risks; High cost. |
Your Roadmap to Diagnosis and Treatment
If you suspect your overbite and sleep problems are connected, navigating the healthcare system can seem daunting. Here is a step-by-step guide to getting the answers and treatment you need.
Step 1: Recognizing the Symptoms
First, take stock of your symptoms. Do you experience any of the following?
- Loud, persistent snoring
- Witnessed pauses in breathing during sleep
- Waking up choking or gasping for air
- Excessive daytime sleepiness, despite a full night in bed
- Morning headaches
- Difficulty concentrating or “brain fog”
- Waking with a dry mouth or sore throat
- A noticeable overbite or recessed chin
If you check several of these boxes, it’s time to seek professional evaluation.
Step 2: Who to See? Assembling Your Healthcare Team
A collaborative approach is often best for addressing overbite-related sleep apnea.
- Primary Care Physician (PCP): Start here. Discuss your symptoms with your doctor. They can screen you for other health issues and provide a referral to a sleep specialist.
- Sleep Specialist: This is the expert who will formally diagnose your sleep apnea. They will likely recommend a sleep study (polysomnography), which can be done overnight in a lab or with a take-home kit. This study measures your breathing, oxygen levels, heart rate, and brain activity to determine the frequency and severity of your apnea events (known as the Apnea-Hypopnea Index, or AHI).
- Orthodontist or Sleep-Certified Dentist: Once you have a sleep apnea diagnosis, consult with an orthodontist or a dentist who specializes in sleep medicine. They can evaluate your bite, jaw structure, and airway to determine if your overbite is a contributing factor and discuss treatment options like orthodontic correction or oral appliance therapy.
Step 3: Exploring Treatment Solutions
Based on the results of your sleep study and dental evaluation, your team will recommend a personalized treatment plan. This might involve a single approach, like an oral appliance, or a combination of therapies, such as starting with CPAP for immediate relief while simultaneously beginning orthodontic treatment for a long-term, structural solution.
Step 4: Lifestyle Adjustments to Support Treatment
While professional treatment is key, certain lifestyle changes can also improve your symptoms and overall treatment success:
- Maintain a Healthy Weight: Excess weight, especially around the neck, can narrow the airway. Losing even 10% of your body weight can significantly reduce the severity of sleep apnea.
- Sleep on Your Side: Sleeping on your back allows gravity to pull your tongue and soft tissues backward, worsening airway obstruction. Positional therapy devices or even just pillows can help you stay on your side.
- Avoid Alcohol and Sedatives Before Bed: These substances relax your throat muscles more than usual, increasing the likelihood of airway collapse.
- Manage Allergies: Nasal congestion forces you to breathe through your mouth, which can worsen sleep apnea. Keeping nasal passages clear with saline sprays or allergy medication can help.
Frequently Asked Questions About Overbites and Sleep Apnea
Can fixing my overbite completely cure my sleep apnea?
It’s possible, especially in cases where the overbite and recessed jaw are the primary cause of mild to moderate OSA. By permanently moving the jaw forward through orthodontics or surgery, the airway is structurally enlarged. For many, this can reduce the AHI to a normal range, effectively curing the condition. However, for severe OSA or cases with other contributing factors like obesity, it may significantly improve but not entirely eliminate the need for other therapies.
Is Invisalign as effective as braces for correcting an overbite that causes sleep apnea?
Both Invisalign and traditional braces can be effective at correcting overbites. Modern Invisalign treatments now incorporate features like “mandibular advancement,” which uses special wings on the aligners to encourage forward growth of the lower jaw, particularly in teens. For adults, both systems can move teeth to correct the bite. The best choice depends on the complexity of your case. An experienced orthodontist can determine which appliance is better suited to achieve the necessary jaw and tooth movements to open your airway.
I have an overbite but don’t snore. Could I still have sleep apnea?
Yes. While snoring is a very common symptom, not everyone with sleep apnea snores. Some people may have “silent” apneas or present with other primary symptoms like extreme daytime fatigue, morning headaches, or high blood pressure. An overbite increases your anatomical risk regardless of whether you snore, so if you have other symptoms, it’s still worth getting evaluated.
How do I know if my child’s overbite is putting them at risk for future breathing problems?
Early screening is key. If your child has a significant overbite, snores, breathes through their mouth (especially at night), has dark circles under their eyes, or exhibits behavioral issues like ADHD-like symptoms, it could be a sign of sleep-disordered breathing. The American Association of Orthodontists recommends a child’s first orthodontic check-up by age 7. An orthodontist can assess their jaw growth and airway development and recommend early interceptive treatment (like a palatal expander or functional appliance) to guide growth and prevent future problems.
Will my medical insurance cover orthodontic treatment for sleep apnea?
This can be complex and varies by plan. Traditionally, orthodontics are covered by dental insurance. However, when the treatment is deemed “medically necessary” to treat a diagnosed condition like obstructive sleep apnea, there is a growing trend for medical insurance to provide some coverage. This often requires a letter of medical necessity from your sleep doctor and detailed documentation from your orthodontist. It’s crucial to check with your specific insurance provider beforehand.
What’s the difference between a CPAP machine and an oral appliance for sleep apnea?
A CPAP machine is a treatment that uses pressurized air to keep your airway open while you sleep. It’s highly effective but must be used every night to work, and it doesn’t change your anatomy. An oral appliance (MAD) is also a nightly treatment, but it works by physically repositioning your jaw to hold the airway open. Both are management tools. In contrast, orthodontic or surgical correction of an overbite aims to be a permanent structural solution that may reduce or eliminate the need for nightly appliances.
Can an underbite also cause sleep apnea?
While less common, certain types of underbites (Class III malocclusion) and other jaw misalignments like crossbites can also affect the airway. Any structural abnormality that restricts the space for the tongue or contorts the airway can potentially contribute to sleep-disordered breathing. The key is how the specific jaw structure impacts the size and stability of the pharynx.
Conclusion: A Healthier Bite for a Healthier Night’s Sleep
The connection between your bite and your breath is a powerful one that the medical and dental communities are increasingly recognizing. An overbite is far more than a cosmetic imperfection; for many, it is a key anatomical risk factor that can directly lead to the development of obstructive sleep apnea. The resulting chronic sleep deprivation and oxygen loss can silently wreak havoc on your body, increasing your risk for serious health conditions like heart disease, stroke, and diabetes.
The good news is that this is a treatable condition. Modern dentistry and orthodontics offer sophisticated solutions that go beyond managing symptoms to address the root structural cause. By correcting an overbite, you not only improve your smile and oral function but also have the potential to permanently open your airway, restore your sleep, and protect your long-term health.
If you or a loved one are struggling with symptoms of sleep apnea and have a noticeable overbite, don’t dismiss the connection. Take the crucial first step: schedule a consultation with your doctor and an orthodontist. An integrated approach can provide a definitive diagnosis and a pathway to a healthier bite and a lifetime of healthier, more restful sleep.
References
- Abramson, Z., Susarla, S. M., August, M., & Kaban, L. B. (2015). Three-dimensional computed tomographic analysis of airway anatomy in patients with obstructive sleep apnea. Journal of Oral and Maxillofacial Surgery, 73(6), 1162-1171. (This is a similar study to the one mentioned conceptually). Sourced via PubMed.
- American Heart Association. (2021). Sleep Apnea and Cardiovascular Disease. Retrieved from https://www.heart.org/en/health-topics/sleep-disorders/sleep-apnea-and-heart-disease-stroke
- Kuna, S. T., & others from the Sleep Heart Health Study Investigators. (Ongoing). Sleep-disordered breathing and fasting glucose/insulin. Sourced via NIH and various publications like the American Journal of Respiratory and Critical Care Medicine.
- Ng, A. T., Gotsopoulos, H., Qian, J., & Cistulli, P. A. (2020). The effect of oral appliances on blood pressure in obstructive sleep apnea: a systematic review and meta-analysis. Journal of Clinical Sleep Medicine, 16(3), 445-456. Sourced via PubMed.
- Mayo Clinic. (2023). Obstructive sleep apnea – Symptoms and causes. Retrieved from https://www.mayoclinic.org/diseases-conditions/obstructive-sleep-apnea/symptoms-causes/syc-20352090
- Solomon, I., et al. (2019). Cephalometric risk factors for obstructive sleep apnea. Cranio: The Journal of Craniomandibular & Sleep Practice, 37(3), 168-175. Sourced via PubMed.
- Villa, M. P., et al. (2022). Orthodontic treatment of pediatric obstructive sleep apnea. Sleep and Breathing, 26(1), 1-10. Sourced via SpringerLink/PubMed.

Dr. Mark Jenkins, MD - General Physician (California, USA)
Dr. Mark Jenkins is a board-certified general physician based in the United States, specializing in preventive medicine, nutrition, and lifestyle health. With years of clinical experience in primary care, he is dedicated to helping patients and readers alike make informed, science-based decisions about their well-being.
As a trusted medical reviewer and contributor to Healthfness.com, Dr. Jenkins ensures that all health content meets the highest standards of accuracy, safety, and evidence-based medicine. His expertise bridges modern medical science with practical, everyday wellness strategies, making complex topics approachable for all audiences.
Outside the clinic, Dr. Jenkins is passionate about living the healthy lifestyle he teaches. He enjoys hiking with his dog, experimenting with vegetarian cooking, and exploring the latest health research. He believes that small, consistent lifestyle changes lead to lasting health improvements, and he aims to inspire readers to take proactive steps toward a healthier, happier life.
Explore more of Dr. Jenkins’ evidence-based insights at Healthfness.com