Before we know about what is Chronic Pancreatitis ICD 10 we should know what is Pancreatitis.
What is Pancreatitis?
Pancreatitis is a medical illness that is experienced when the pancreas, a gland located behind the stomach, becomes inflamed. The pancreas plays an important role in the digestion of food by producing enzymes that help break down food in the small intestine, as well as hormones that regulate blood sugar levels. Here we will go through ICD-10 code for chronic Pancreatitis.
There are two main types of pancreatitis:
Acute Pancreatitis: Acute pancreatitis is a sudden inflammation of the pancreas.
Chronic Pancreatitis: Chronic pancreatitis is a long-term inflammation of the pancreas.
Research work on Chronic Pancreatitis ICD 10
Chronic Pancreatitis ICD 10 is a serious medical disorder that can damage the pancreas permanently, limiting its capacity to generate digestive enzymes and hormones such as insulin. We shall now look at various studies on Chronic Pancreatitis ICD-10.
One study published in Scientific Reports examined Chronic Pancreatitis ICD 10 and cancer risk in a matched cohort study using national claims data in South Korea here they discover the link between Chronic Pancreatitis and cancer.
Here is another study by journals lww where they explore The Epidemiology of Alcohol-Induced Pancreatitis where they examined the association between alcohol and pancreatitis but the precise magnitude of alcohol’s impact remains unknown.
Different ICD-10 Code For Chronic Pancreatitis
Here are the main kinds of chronic pancreatitis and their related ICD-10 codes:
- Obstructive chronic pancreatitis: ICD-10 code K86.1
- Alcohol-induced chronic pancreatitis: ICD-10 code K86.0
- Idiopathic chronic pancreatitis: ICD-10 code K86.8
- Hereditary chronic pancreatitis: ICD-10 code K86.3
- Recurrent acute pancreatitis with chronic pancreatitis: ICD-10 code K86.2
Obstructive chronic pancreatitis ICD-10
Obstructive chronic pancreatitis is a kind of chronic pancreatitis caused by an obstruction in the pancreatic duct, which inhibits digestive enzymes from properly flowing and causes pancreatic inflammation. Gallstones, tumors, scar tissue, or other abnormalities in the pancreas or surrounding organs can all cause the blockage.
Alcohol-induced chronic pancreatitis ICD-10
Chronic pancreatitis caused by long-term alcohol usage is known as alcohol-induced chronic pancreatitis. It is distinguished by pancreatic inflammation and scarring, which can impede the organ’s capacity to produce digesting enzymes and hormones such as insulin. The ICD10 code for alcohol-induced chronic pancreatitis is K86.0
Idiopathic chronic pancreatitis ICD-10
Idiopathic chronic pancreatitis is a kind of chronic pancreatitis that has no apparent underlying illness or etiology. It is distinguished by pancreatic inflammation and scarring, which can impede the organ’s capacity to produce digesting enzymes and hormones. ICD 10 code for idiopathic chronic pancreatitis is K86.8 in the ICD-10 coding system, which is a subcategory of chronic pancreatitis.
Hereditary chronic pancreatitis ICD-10
Hereditary chronic pancreatitis is a kind of chronic pancreatitis that is passed down via families. Hereditary chronic pancreatitis is coded as K86.1, which is a subset of chronic pancreatitis in the ICD-10 classification system. Mutations in specific genes that are passed down through families cause hereditary chronic pancreatitis.
Recurrent acute pancreatitis with chronic pancreatitis ICD-10
Recurrent acute pancreatitis with chronic pancreatitis is a form of pancreatitis that includes both acute and chronic pancreas inflammation. A person with this disorder has recurring episodes of acute pancreatitis, which can eventually lead to chronic inflammation and pancreatic damage. Recurrent acute pancreatitis with chronic pancreatitis is coded as K86.2 in the ICD-10 classification system.
Chronic Pancreatitis ICD 10 causes
Chronic pancreatitis is a disorder in which the pancreas slowly gets inflamed and damaged. Chronic pancreatitis is designated as category K86 in the ICD-10 classification system, which has several subgroups dependent on the underlying cause of the illness.
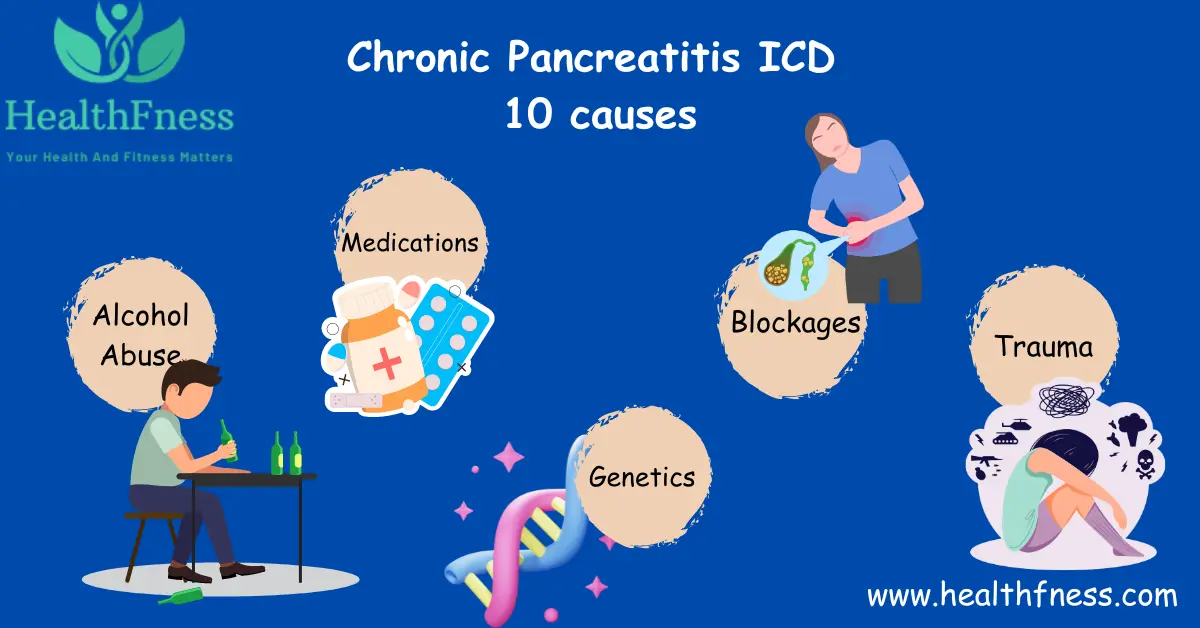
Chronic pancreatitis can have a variety of reasons, however, the following are some of the most common:
Alcohol abuse: Continually drinking alcohol is a major cause of chronic pancreatitis because it damages pancreatic tissue and impairs its capacity to function normally.
Genetics: Gene changes can potentially cause chronic pancreatitis, especially in cases of hereditary chronic pancreatitis.
Autoimmune disorders: Certain autoimmune disorders, such as autoimmune pancreatitis, can lead to ongoing pancreatic inflammation.
Blockages: Blockages in the pancreatic duct or bile duct can cause in digestive juice backup and pancreatic inflammation.
Trauma: Abdominal traumas, such as those received in vehicle accidents or sports injuries, can injure the pancreas and cause chronic inflammation.
Medications: Some medications, such as chemotherapy therapies, can cause pancreatic inflammation and damage.
Unknown causes: The underlying cause of chronic pancreatitis may be unknown in some circumstances.
Signs and Symptoms of Chronic Pancreatitis ICD-10
Chronic pancreatitis symptoms can differ between individuals, but some common ones are:
Abdominal pain
Abdominal discomfort is often the most apparent symptom of chronic pancreatitis. The pain could be dull or intense, and it could be in the upper abdomen or back.
Digestive problems
Chronic pancreatitis can produce a range of digestive issues, including nausea, vomiting, diarrhea, and oily or greasy feces. This is because the pancreas does not produce enough digestive enzymes to properly digest food.
Weight loss
Because of improper nutrient absorption, chronic pancreatitis can cause weight loss.
Diabetes:
In some cases, chronic pancreatitis can damage insulin-producing cells in the pancreas, resulting in diabetes.
Jaundice
When the pancreatic tract is blocked, bilirubin builds up in the blood, causing yellowing of the skin and eyes.
Fever
In some circumstances, chronic pancreatitis can develop into a low-grade fever.
It is important to keep in mind that not all people with chronic pancreatitis will have all of these symptoms, and some may have additional symptoms that aren’t listed here.
Diagnosis of Chronic Pancreatitis ICD-10
The diagnosis of chronic pancreatitis typically involves:
Medical history
A doctor would often inquire about the patient’s symptoms, such as when they began, how severe they are, and whether there are any things that make them worse or better.
Physical examination
A doctor may do a physical examination to look for symptoms of pancreas inflammation or injury, such as discomfort or swelling in the belly.
Imaging tests
Imaging tests, such as computed tomography (CT) scans, magnetic resonance imaging (MRI) scans, and ultrasound can aid in the visualization of the pancreas and the detection of any abnormalities such as inflammation, scarring, or calcifications.
Laboratory tests
Blood tests can be done to look for high levels of pancreatic enzymes like amylase and lipase. Additional blood tests may be performed to look for underlying reasons for Chronic Pancreatitis, such as high triglyceride levels or autoimmune antibodies.
Treatment of Chronic Pancreatitis ICD-10
The treatment of chronic pancreatitis may involve a combination of:
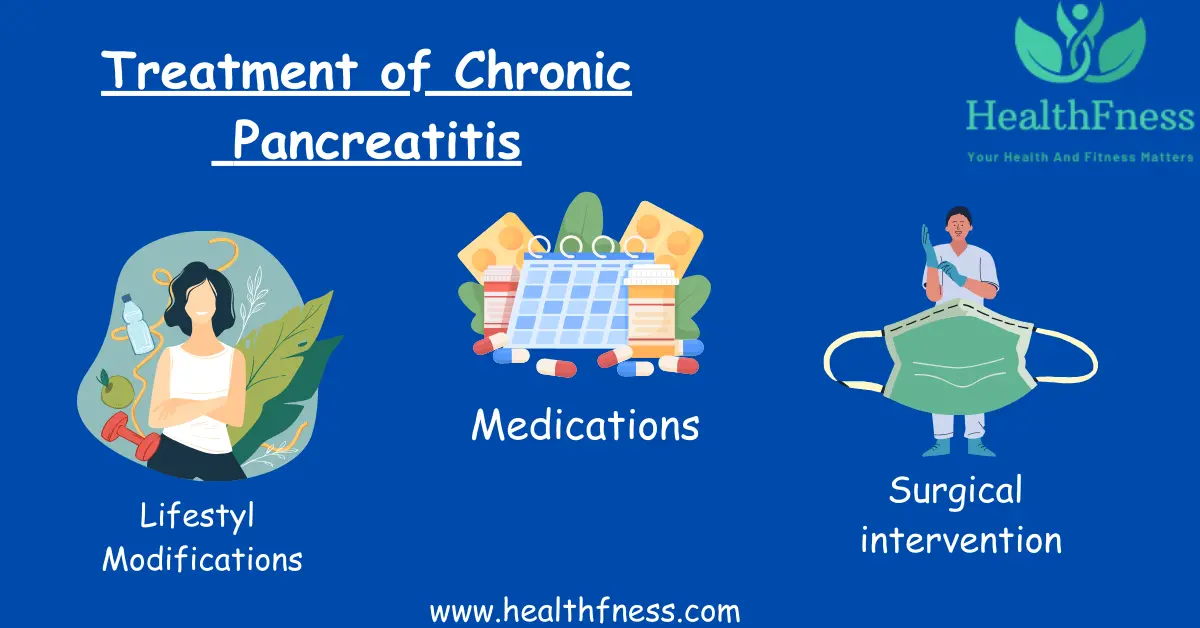
Lifestyle modifications
Individuals with chronic pancreatitis may benefit from making dietary and lifestyle changes. This could include avoiding alcohol and tobacco, eating smaller, more frequent meals, and avoiding foods heavy in fat or difficult to digest.
Medications
Medications may be used to control symptoms or avoid the consequences of chronic pancreatitis, depending on the underlying cause. Nonsteroidal anti-inflammatory medications (NSAIDs), acetaminophen, and opioids may be used to treat pain.
Surgical intervention
Surgical intervention may be required in some cases to manage complications or improve symptoms. In some cases, endoscopic therapy, pancreatic duct drainage, or surgical removal of the pancreas may be recommended.
Follow-up care
To treat symptoms and prevent complications, patients with chronic pancreatitis require continuous monitoring and follow-up care. Frequent visits to a healthcare professional, imaging exams, and blood tests may be required to evaluate the condition’s course and alter treatment as appropriate.
Prevention of Chronic Pancreatitis ICD 10
Chronic pancreatitis prevention is decreasing or eliminating risk factors that can contribute to the condition’s development. Some preventive actions that can be implemented are as follows:
Avoiding alcohol: Because alcohol is a key cause of chronic pancreatitis, restricting or eliminating alcohol usage can dramatically lower the risk of getting the condition.
Maintaining a healthy weight: Obesity is another risk factor for chronic pancreatitis; therefore, keeping a healthy weight with a balanced diet and regular exercise will help prevent the illness.
Avoiding certain medications: Some drugs, such as corticosteroids and certain antibiotics, can increase the chance of developing chronic pancreatitis. Individuals should discuss the potential hazards and advantages of any medications they are taking with their healthcare professionals.
Getting regular check-ups: Frequent check-ups with a healthcare professional can help with the detection of potential risk factors for chronic pancreatitis and allow for early intervention and treatment.
FAQS
Conclusion
Finally, chronic pancreatitis is a complex condition that is coded as K86 in the ICD-10 system. It can be caused by a variety of circumstances. Chronic pancreatitis is diagnosed using clinical symptoms, imaging scans, and laboratory tests. Prevention of chronic pancreatitis involves minimizing risk factors such as alcohol consumption, maintaining a healthy diet, and avoiding exposure to toxins.
Video Credits:

Dr. Mark Jenkins, MD - General Physician (California, USA)
Dr. Mark Jenkins is a board-certified general physician based in the United States, specializing in preventive medicine, nutrition, and lifestyle health. With years of clinical experience in primary care, he is dedicated to helping patients and readers alike make informed, science-based decisions about their well-being.
As a trusted medical reviewer and contributor to Healthfness.com, Dr. Jenkins ensures that all health content meets the highest standards of accuracy, safety, and evidence-based medicine. His expertise bridges modern medical science with practical, everyday wellness strategies, making complex topics approachable for all audiences.
Outside the clinic, Dr. Jenkins is passionate about living the healthy lifestyle he teaches. He enjoys hiking with his dog, experimenting with vegetarian cooking, and exploring the latest health research. He believes that small, consistent lifestyle changes lead to lasting health improvements, and he aims to inspire readers to take proactive steps toward a healthier, happier life.
Explore more of Dr. Jenkins’ evidence-based insights at Healthfness.com