A form of anemia called microangiopathic hemolytic anemia (MAHA) is characterized by way of hemolysis the breakdown of red blood cells inside tiny blood vessels. It often entails the development of blood clots inside these veins, which worsens hemolysis.
MAHA is critical due to the fact, that if untreated, it could result in good-sized morbidity and mortality. Anaemia ↗is introduced with the aid of the breakdown of crimson blood cells and can result in weak spots, exhaustion, and breathlessness which disturb the general first-rate of a person’s life. When MAHA is intense, it can result in organ failure or damage, stroke, or maybe death. For better results, MAHA must be controlled and recognized early.
Microangiopathic Hemolytic Anemia ICD 10
Microangiopathic Hemolytic Anemia ICD 10 code is D59.4.This code is used to perceive cases of MAHA in medical information. It is utilized by healthcare professionals, docs, and companies for monitoring and evaluation functions and facilitates preserving records of clinic bills.
The D59.4 code is further broken down into subcategories or subgroups based totally on the motive of the MAHA. For example, D59.41 is used for MAHA due to an infection, which includes Shiga toxin-producing Escherichia coli (STEC) or Streptococcus pneumoniae. D59.42 is used for MAHA as a result of medicinal drugs or pills, inclusive of chemotherapy or quinine.
D59.43 is used for MAHA because of autoimmune disorders. It means the code will barely exchange consistent with the purpose that advanced MAHA.
Microangiopathic Hemolytic Anemia Causes
Here are some of the common causes of MAHA:
Thrombotic microangiopathy (TMA)
Thrombotic microangiopathy (TMA) is a disorder wherein the microvasculature develops tiny blood clots (microthrombi). Numerous conditions and medicines, which include chemotherapy and immunosuppressive capsules, bacterial infections like Shiga toxin-producing Escherichia coli (STEC) and Streptococcus pneumonia, autoimmune diseases like systemic lupus erythematosus (SLE), and pregnant-associated problems like preeclampsia and HELLP syndrome can all contribute to TMA.
Disseminated Intravascular Coagulation (DIC)
DIC is a circumstance wherein the body’s ordinary blood clotting mechanisms come to be overactive and lead to the formation of small blood clots during the frame. These clots can consume clotting elements and platelets, leading to bleeding issues and the destruction of purple blood cells. DIC can be a result of a selection of factors, together with sepsis, trauma, and cancer.
Hemolytic Uremic Syndrome (HUS)
HUS is a condition characterized by the formation of small blood clots in the microvasculature of the kidneys, main to kidney harm and the destruction of purple blood cells. HUS is maximum normally because of contamination with a pressure of Escherichia coli bacteria called E. Coli O157:H7, although different infectious and non-infectious causes have also been pronounced.
Malignant Hypertension
An extreme form of excessive blood pressure that could cause the development of tiny blood clots within the microvasculature of the kidneys, brain, and other organs is called malignant high blood pressure. Red blood mobile loss of life and tissue damage might also result from this.
HELLP Syndrome
Hemolysis, multiplied liver enzymes, and a low platelet are all characteristics of the pregnancy situation known as HELLP syndrome. It can bring about the demise of crimson blood cells in the microvasculature and is notion to be added on by using an aberrant blood vessel hobby.
Antiphospholipid Syndrome (APS)
Antiphospholipid syndrome (APS) is an autoimmune contamination wherein specific blood proteins are attacked by way of the body’s immune machine, inflicting blood clots and other difficulties. Small blood clots that shape due to APS can damage the tissue and kill red blood cells using obstructing the microvasculature.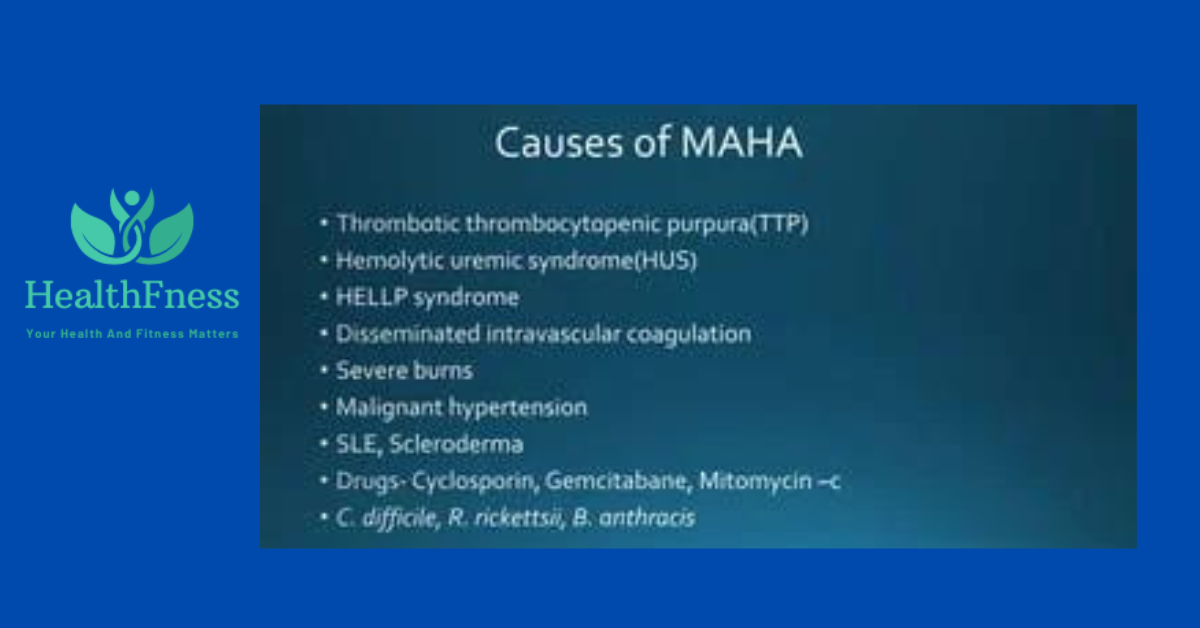
Other Causes
Other elements Infections like malaria and babesiosis, capsules like quinine and ticlopidine, and inherited sicknesses like abnormal hemolytic uremic syndrome (aHUS) and hereditary thrombotic thrombocytopenic purpura (hTTP) are a number of the less common reasons of Microangiopathic Hemolytic Anemia (MAHA).
Microangiopathic Hemolytic Anemia Symptoms
The symptoms of Microangiopathic Hemolytic Anemia (MAHA) can vary from person to person because of the different causes of developing this disease. However, some common symptoms of MAHA include:
- Fatigue_ Anemia as a result of the destruction of red blood cells can cause fatigue and weakness. An individual feels fatigued continuously all through this contamination.
- Jaundice_ The destruction of crimson blood cells can cause an accumulation of bilirubin, a pigment that causes yellowing of the skin and eyes.
- Dark urine_The breakdown of crimson blood cells can lead to the production of hemoglobin, which can be excreted within the urine and cause it to appear dark or tea-colored not like ordinary urine.
- Abdominal pain_ A Few instances of MAHA can lead to the formation of blood clots or accumulation of blood in the small blood vessels of the gastrointestinal tract, leading to stomach ache.
- Neurological symptoms_ In Severe instances of MAHA, result in the formation of blood clots inside the small blood vessels of the mind and may result in neurological signs along with confusion, seizures, and coma, and have an effect on a person’s life badly.
- Kidney dysfunction_MAHA can cause kidney dysfunction because of the formation of blood clots inside the small blood vessels of the kidneys.
Its method could create blood clots in vessels all over the frame. Blood clots forestall the blood from drifting in the body which ends up in risky headaches.
Diagnosis Of Microangiopathic Hemolytic Anemia
The diagnosis of MAHA includes numerous tests that figure out the cause of this disease and also help to see the extent of organ damage.
Medical History Review And Physical Exam
To locate any Microangiopathic Hemolytic Anemia (MAHA) signs and symptoms or signs and symptoms, along with jaundice, abdominal soreness, or neurological signs and symptoms, the physician will assess the affected person’s medical records and conduct a physical examination.
Laboratory Tests
Blood exams could be prescribed to test the levels of hemoglobin, pink blood cells, and different blood elements. Red blood cellular and hemoglobin ranges are regularly diminished in MAHA, and the number of reticulocytes (immature purple blood cells) may additionally upward push. Schistocytes, which might be damaged-up pink blood cells, can also be located on a blood smear.
Coagulation Tests
Blood clotting assessments may be ordered to evaluate the affected person’s danger of growing blood clots, which may be a worry of MAHA. These tests can consist of prothrombin time (PT), activated partial thromboplastin time (aPTT), and fibrinogen ranges.
Kidney Function Tests
Microangiopathic Hemolytic Anemia (MAHA) can cause kidney disorders, so tests to assess kidney characteristics can be ordered, inclusive of blood urea nitrogen (BUN) and creatinine levels.
Imaging Tests
Imaging exams can be ordered to assess the volume of organ damage and to pick out any blood clots. These checks can encompass ultrasound, computed tomography (CT) scan, or magnetic resonance imaging (MRI).
Underlying Cause Evaluation
Depending on the results of the above tests, further testing may be needed to identify the underlying cause of the MAHA, such as an infection or autoimmune disorder.
This series of tests helps to find which treatment course is best for the patient.
Microangiopathic Hemolytic Anemia Treatment
The remedy of Microangiopathic Hemolytic Anemia ↗(MAHA) relies upon many factors and treatment goals to halt the destruction of pink blood cells, manage signs, and prevent complications.
- Treating the underlying reason_ Microangiopathic Hemolytic Anemia (MAHA) results from an infection, remedy, or autoimmune sickness, treating the root motive is essential to prevent the destruction of purple blood cells. This can also contain antibiotics, discontinuing medicinal drugs, or immunosuppressive therapy.
- Blood Transfusions_ In situations with extreme MAHA, blood transfusions can be required to replenish the purple blood cells that have been lost and to decorate the supply of oxygen to the frame’s tissues.
- Plasma Exchange_ Plasma change can be achieved to put off the antibodies from the blood and reduce the death of purple blood cells in some instances of MAHA brought on through an autoimmune illness. This hospital treatment is terrific.
- Dialysis_ Dialysis may be required to filter out the blood, dispose of greater fluids, and cleanse the frame of waste items if MAHA causes a kidney ailment.
- Surgery_ Surgery can be required in rare instances to do away with blood clots or damaged tissue.
- Close Monitoring_ Patients with Microangiopathic Hemolytic Anemia (MAHA) need to have their blood counts, organ functions, and remedy responses intently monitored. It might be required to timetable ordinary compliance with-up sessions and laboratory trying out to display any problems and gauge the performance of the remedy.
The remedy for Microangiopathic Hemolytic Anemia is complex and frequently calls for a multidisciplinary method concerning hematologists, nephrologists, and different specialists.
FAQs
What is microangiopathic hemolytic anemia (MAHA)?
A: Microangiopathic hemolytic anemia (MAHA) is a form of anemia characterized by using the strange destruction of crimson blood cells because of their passage through small blood vessels that are broken or obstructed.
What reasons microangiopathic hemolytic anemia?
MAHA can be caused by diverse underlying situations, together with thrombotic thrombocytopenic purpura (TTP), hemolytic uremic syndrome (HUS), disseminated intravascular coagulation (DIC), malignant high blood pressure, and sure autoimmune issues.
What are the signs of microangiopathic hemolytic anemia?
Symptoms of MAHA may additionally encompass fatigue, weak point, shortness of breath, faded pores and skin, jaundice (yellowing of the skin and eyes), darkish urine, and an multiplied coronary heart rate.
How is microangiopathic hemolytic anemia diagnosed?
Diagnosis of MAHA commonly entails a mixture of medical history evaluate, bodily exam, blood checks (such as whole blood be counted and peripheral blood smear), and occasionally additional diagnostic checks such as bone marrow biopsy or imaging research.
What are the remedy alternatives for microangiopathic hemolytic anemia?
Treatment of MAHA relies upon at the underlying purpose. It can also contain addressing the number one circumstance, managing symptoms, and in a few instances, interventions along with plasma change, corticosteroids, immunosuppressive remedy, or blood transfusions can be essential.
Reference
Read this report for more information-Diagnostic approach to microangiopathic hemolytic disorders
The conclusion of this study is Thrombotic microangiopathies (TMAs) embody a spectrum of issues characterized with the aid of thrombocytopenia, microangiopathic hemolytic anemia, and organ damage. While classical conditions like thrombotic thrombocytopenic purpura (TTP) and hemolytic-uremic syndrome (HUS) were well-described, enhancements in expertise have delivered approximately the recognition of super subtypes with numerous etiologies, together with supplement-mediated TMAs, drug-addled approximately TMAs, metabolism-mediated TMAs, and coagulation-mediated TMAs.
The laboratory performs an important function in diagnosing the disorders, with checks for ADAMTS13 interest, complement factors, genetic mutations, and specific antibodies being critical for proper evaluation. Treatment techniques have advanced, with centered restoration techniques along with plasma alternate, anticomplement remedy (e.g., eculizumab), and supportive care tailored to the underlying cause of the TMA.
Overall, improvements in our information on TMAs have induced advanced diagnostic accuracy and treatment effects, underscoring the significance of ongoing research and collaboration among clinicians and laboratory experts in managing these complicated disorders.
Conclusion
In conclusion, Microangiopathic Hemolytic Anemia (MAHA) is an unprecedented but severe medical situation characterized with the aid of the destruction of crimson blood cells and the formation of blood clots in the small blood vessels. MAHA will have loads of underlying causes, which include infections, autoimmune issues, and medicinal drugs.
The prognosis of MAHA entails an aggregate of laboratory tests, imaging research, radical clinical records, and physical examination. Treatment options rely upon the underlying motive of the situation and may involve blood transfusions, plasma exchange, medicines, dialysis, and surgical operations. Regular tracking and follow-up appointments are essential to manipulate signs and symptoms and investigate remedy effectiveness.
Video Credits:

Dr. Mark Jenkins, MD - General Physician (California, USA)
Dr. Mark Jenkins is a board-certified general physician based in the United States, specializing in preventive medicine, nutrition, and lifestyle health. With years of clinical experience in primary care, he is dedicated to helping patients and readers alike make informed, science-based decisions about their well-being.
As a trusted medical reviewer and contributor to Healthfness.com, Dr. Jenkins ensures that all health content meets the highest standards of accuracy, safety, and evidence-based medicine. His expertise bridges modern medical science with practical, everyday wellness strategies, making complex topics approachable for all audiences.
Outside the clinic, Dr. Jenkins is passionate about living the healthy lifestyle he teaches. He enjoys hiking with his dog, experimenting with vegetarian cooking, and exploring the latest health research. He believes that small, consistent lifestyle changes lead to lasting health improvements, and he aims to inspire readers to take proactive steps toward a healthier, happier life.
Explore more of Dr. Jenkins’ evidence-based insights at Healthfness.com